Knee Replacement Surgery for the Recreational Athlete
Aug 22, 2019Richard A. Sweet, M.D. (Retired 2022)
Kate S. Hamilton, PA-C
INTRODUCTION:
In the early days of total knee replacement (TKR) surgery, the goal of the procedure was to provide a knee that allowed an elderly patient disabled with arthritis of the knee to walk comfortably for the purpose of pursuing activities of daily living. In recent years these modest goals have dramatically changed. The aging baby boomer generation has expectations of maintaining an active and athletic lifestyle well into the later years of life. And ever younger patients with knee arthritis severe enough to interfere with participation in sports are demanding a surgical solution to their problem. To meet these societal demands and expectations, advances in knee replacement implant designs and surgical techniques have evolved. As a result, it is now possible for patients receiving knee (and hip) replacement surgery to lead active lifestyles and to continue to participate in recreational sports and vigorous exercise programs.
CHALLENGES IN TKR SURGERY FOR THE ATHLETIC PATIENT
Unique challenges are faced by the surgeon in providing a stable knee that will respond to peak demands of athletics. These include:
- LOSS OF THE ANTERIOR CRUCIATE LIGAMENT (ACL):Though in recent years there has been an attempt to design an ACL sparing knee replacement, these efforts have thus far either led to outright failure or are as yet unproven. In all clinically successful total knee replacement designs, the anterior cruciate ligament is sacrificed. The loss of the ACL creates challenges for the surgeon to build a new knee for the active patient that will be sufficiently stable so as to withstand the stresses of vigorous exercise, strenuous work demands, and athletic activities.
- MAINTENANCE OF “PERFECT” POSTERIOR CRUCIATE LIGAMENT (PCL) FUNCTION:Posterior knee stability (prevention of the tibia from sliding back under the femur) is crucial to the function of the knee in all active knee replacement patients. In the normal knee, the PCL (located behind the ACL in the center back of the knee) performs this function. Normal PCL function is essential for athletic movements such as jumping, pivoting, quick starting and stop- ping, and even for more routine activities such as stair climbing and kneeling. The PCL (as op- posed to the ACL) is not always removed in TKR surgery. In PCL Retaining implants, stability is dependent on the surgeon’s experience and skill in properly preserving, tensioning and balanc- ing the PCL. If the PCL is too loose, posterior laxity makes participation in sports difficult. If it is balanced too tightly, the ability to gain knee flexion is compromised. In PCL Sacrificing implants, posterior stability is an inherent part of the design but at a cost of sacrificing / removing more bone from the femur and placing more stress on the cement bond of the implants to the bone (due to this bone loss, PCL sacrificing implants are also significantly more difficult to revise, should the future need ever occur). The bottom line, for a TKR patient to remain athleti- cally active, near perfect posterior stability must be maintained, either by the surgeons balancing and tensioning of the patients own PCL or by substituting for it via PCL sacrificing implant design. There are advantages and disadvantages to each strategy.
- COLLATERAL LIGAMENTS BALANCED:The medial and lateral collateral ligaments on the inside and outside of the knee must be evenly balanced and properly tensioned to provide side-to-side stability. In the process, preoperative mal-alignment such as “bowed” or “knock- kneed” deformity must be corrected.

FIGURES 1, 2 & 3. The PCL (blue arrow) may be sacrificed or preserved. If sacrificed, the post (yellow arrow) of the tibial plastic insert abuts against a metal bar (red arrow) of the femur to provide posterior stability.
MUSCLE PRESERVING (MINIMALLY INVASIVE) SURGICAL APPROACH FOR THE ATHLETE
For a rapid return to a high demand lifestyle, it is crucial that the surgical approach avoids cutting into the quadriceps muscle. This includes not only returning to athletics, but also to a high demand job or a vigorous exercise program. Experienced surgeons focused on and trained in quadriceps sparing minimally invasive surgical techniques can utilize this surgical approach in virtually all patients.
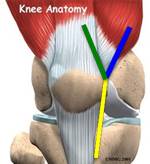 The YELLOW line represents the distal incision into the joint common to all surgical approaches of the knee. The GREEN proximal extension of this yellow line represents the standard surgical approach into the joint that cuts into the quadriceps tendon and muscle, which delays recovery. The BLUE extension of the incision represents the Quadriceps Sparing approach that allows for immediate return of quadriceps function speeding rehab for the athletic patient.
The YELLOW line represents the distal incision into the joint common to all surgical approaches of the knee. The GREEN proximal extension of this yellow line represents the standard surgical approach into the joint that cuts into the quadriceps tendon and muscle, which delays recovery. The BLUE extension of the incision represents the Quadriceps Sparing approach that allows for immediate return of quadriceps function speeding rehab for the athletic patient.
RECOVERY TIMELINE FOR THE ATHLETIC PATIENT
- Hospital stay 1 night (some surgeons are doing outpatient surgery – I still like to watch patients overnight to make sure all is going well immediately post op)
- Physical therapy starts the day of surgery, with a vigorous therapy session the first day after surgery before being discharged
- Full weight bearing from the beginning. Off the walker / crutches as soon as tolerated, often after just a few days.
- Physical therapy (home and outpatient) for 6 weeks
- Exercise program to maintain leg strength recommended indefinitely.
- Light recreational sports allowed at 6 weeks post op
- Vigorous sports / activities at 3 months’ post op
RECREATIONAL SPORTS & EXERCISE OPTIONS FOR TKR PATIENTS
General Instructions:
Most adult recreational athletic activities and exercise programs are possible in knee replacement patients. Activities that subject the knee to excess wear, impact, or risk of injury can shorten the goal of the knee lasting 2-3 decades. Brisk walking, exercise bikes, elliptical trainers, and treadmills are good aerobic substitutes for a running program. Stair climbing machines and the use of excessive weight on leg strengthening machines can sometimes create soreness and swelling in the knee. A resistive leg strengthening exercise program should be of a low weight – high repetition (30 reps or more) strategy. Most fitness class exercise programs are well tolerated, though “step” classes and those emphasizing the repetitive use of the “lunge” position can cause patellar soreness.
Sport Specific Instructions:
With regard to participation in recreational sports, some judgement should be employed. Sports with a high risk of ligament injury to the knee should probably be avoided, as the consequences of such an injury are much greater (often leading to revision surgery). Tennis (especially doubles) and other racquet sports are well tolerated. Biking, even competitively, also is well tolerated. Golfing, even walking the course, should not be a problem. Patients should be able to participate in a vigorous exercise program. An experienced snow skier can resume their sport. Horseback riding is permissible. For the most part, returning to sports is a common-sense decision based on what a patient can tolerate without concerns for “damaging” the knee.



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.