Total Shoulder Replacement – (The “Other” Joint Replacement)
Aug 22, 2019Scott D. Kuiper, M.D.
Even healthy and athletic people can develop arthritis. Sometimes it develops as a result of old traumatic injuries or from the degenerative wear and tear of overuse. Many people know someone with arthritis of their knee or hip who has been treated with an artificial joint replacement. These successful procedures are now performed more frequently than ever. Less common, but just as successful as a pain relieving procedure, is a total shoulder replacement.
THE PROBLEM
The shoulder is a ball-and-socket joint that helps position the hand in space. The ball (humeral head) and socket (glenoid) are covered with a durable, smooth surface called articular cartilage, which forms a protective cushion between the two bones. If this layer of cartilage is damaged from trauma or wears away because of osteoarthritis or degenerative joint disease, the shoulder becomes painful and stiff. The ability to reach, lift, push and pull are greatly diminished, making common activities such as reaching into a back pocket or combing hair very difficult. Recreational activities such as golf and tennis become almost impossible. Sleeping on the affected side is painful,resulting in frequent sleep disturbance.
Figure 1 (right): Shoulder x-ray showing severe arthritis between the Humeral Head (HH) and the Glenoid (G). Figure 2 (left): X-ray of Total shoulder Prosthesis. 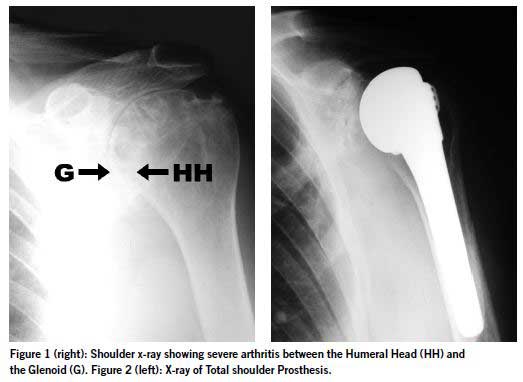
EARLY TREAMTMENT
The first step in treating a painful,stiff shoulder is to see your doctor,who will obtain a detailed history and perform a physical exam. Common complaints include grinding and popping in the shoulder, pain with use and decreased reach. X-rays are used to view the shoulder bones and joint structure to help determine the cause of the problem. Occasionally an MRI is obtained to evaluate the tendons (rotator cuff) surrounding the shoulder.
Initial treatment of shoulder arthritis involves strengthening exercises for the shoulder, anti-inflammatory medications and occasionally an injection of corticosteroid medication. If pain continues despite these measures, you will generally be referred to an orthopedic surgeon who specializes in this type of surgery.
An orthopedic surgeon will review the patient’s age and activity level, as well as the severity of their arthritis. Some people can be treated arthroscopically with a pencil-sized camera and micro shavers to wash, clean and shave the damaged arthritic tissues. In severe cases however, total shoulder replacement is recommended.
WHAT IS TOTAL SHOULDER REPLACEMENT?
Shoulder replacement surgery replaces the damaged joint surfaces with artificial parts called prostheses to relieve pain. The humeral component replaces the damaged ball. A rounded half ball made of metal alloy is attached to a stem that fits securely into the center of the bone. Bone cement is sometimes used to further strengthen this bond. The glenoid component replaces the damaged surface of the socket. This component is a smooth, semi-curved disc of ultrahigh-density polyethylene with a fin or pegs that is cemented or secured to the glenoid surface. The components come in a variety of shapes and sizes to fit each patient’s anatomy (Figure 4). A successful replacement creates a stable, smooth, gliding joint surface that greatly reduces pain and improves the function of the patient’s shoulder.
WHAT IS THE SURGERY AND RECOVERY LIKE?
The incision is made on the front of the shoulder and is three to five inches long. The surgery takes about two hours to perform. When you awaken your arm will be in a sling, but we encourage early range of motion of the arm for activity. While you are in the hospital a physical therapist will give you detailed exer-cise instructions. Most patients only spend one or two nights in the hospital and can leave when they are comfortable on oral pain medicine. Full return to normal activities takes two to three months.
WHAT ARE THE RISKS OF SHOULDER REPLACEMENT?
While shoulder replacement is statistically very safe, complications may occur. These include infection, which if serious, could result in implant removal. Your surgeon will take several precautions to reduce this risk.Loosening of the prosthetic implant can occur over time. Great care is taken to obtain a secure fit in the bone to reduce this risk. Nerves and blood vessels that run close to the joint are retracted to visualize the shoulder. Even when great care is taken, temporary or permanent damage to these structures can occur.
CASE EXAMPLE
J.J.is a 63-year-old right-hand-dominant farmer from Shelbyville, Kentucky. He presented to my office with pain in his left shoulder, which affected his daily activities and caused frequent sleep disturbances.He wanted to continue to enjoy an active lifestyle on his farm. He was sent to me after nonsurgical treatments failed to help his symptoms. My exam demonstrated that his shoulder had good strength in his rotator cuff muscles but extremely limited range of motion. If his shoulder was moved too far in any direction it was very painful. X-rays confirmed severe osteoarthritis (Figure 1).
J.J. had a successful total shoulder replace-ment with an uncemented humeral component and cemented three-peg glenoid component (Figure 2). After one night in the hospital he went home with instructions to do exercises under the guidance of a local physical thera-pist. At three months postoperative he had regained nearly all of his shoulder reach (Figure 3) with good strength and function.


CONCLUSION
Shoulder replacement surgery is a safe and effective solution for improving function and relieving pain in active patients who suffer from arthritis of the shoulder. Many people can resume activities of daily living previously not possible because of the pain and limited reach caused by the arthritic condition of the shoulder.
Dr. Kuiper is a board-certified orthopedic surgeon in pri-vate practice with the Louisville Orthopedic Clinic. After his residency at the University of California,San Diego, he completed an Orthopedic Sports Medicine Fellowship with Dr. James R. Andrews in Birmingham, Alabama. He is an orthopedic consultant with Spalding University and team physician for DuPont Manual High School and Sacred Heart Academy. Dr. Kuiper is a member of the Kentuckiana HealthFitness Editorial Advisory Board.



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.