The Ankle Sprain That Won’t Get Better
Aug 21, 2019George Edward Quill, M.D. (Retired 2023)
With springtime in Louisville upon us, the primary care physician and the orthopaedist alike can expect to see more than his or her fair share of ankle sprains. This is an injury that of course occurs year round, but seems to occur much more frequently this time of year.
It is estimated that approximately 25,000 people in America sprain their ankle every day. These are not always simple injuries and can result in residual symptoms in up to 40 percent of patients. In more than 85 percent of ankle sprains, it is the lateral collateral ligaments (the anterior talofibular and calcaneofibular) that are effected. Less common are injuries to the medial structures, including the deltoid ligament and posterior tibial tendon.
Patients who sustain these ankle sprains present with pain over the injured ligaments, loss of function, and swelling. A severe sprain may be diagnosed in patients who report hearing or feeling a popping sensation, followed by immediate swelling and the inability to walk or finish their athletic endeavor after an inversion injury. It is important to ask the patient if he or she has a history of frequent ankle sprains or giving way as the presenting episode may represent an acute injury superimposed upon chronic ankle instability. This is a more significant injury and often necessitates referral for consideration of lateral ankle ligament reconstruction.
Patients who present with a history of ankle locking or sudden, paroxysmal deep ankle pain, not necessarily any worse on uneven ground than it is on level, may also have an intraarticular loose body necessitating surgical intervention.
Physical examination commonly reveals ecchymosis and swelling around the entire ankle joint, and not just the lateral side. In my experience, the patient with a “goose egg” type of swelling localized only anterolateral often has a better prognosis after ankle inversion injury than the one with diffuse or seemingly insignificant swelling because the latter patient often has a complete ligamentous and capsular tear, allowing dissipation of hematoma and edema throughout the limb.
Tenderness directly localizable to the anterior talofibular, calcaneofibular, or posterior talofibular ligaments helps support the diagnosis of inversion ankle sprain. The examiner must also palpate with one finger the lateral and medial malleoli and the base of the fifth metatarsal to rule out fracture of these structures. It is also very important to examine the entire leg, including the tibiofibular syndesmosis and the proximal fibula as high ankle sprains and proximal fibular fractures can easily be missed.
A test specific for tibiofibular syndesmosis injury is called the squeeze test. This test is performed by compressing the tibia and fibula at the mid calf and then gently dorsiflexing and externally rotating the foot at the level of the ankle. A positive test, indicated by the presence of pain over the distal tibiofibular junction, identifies injury to the syndesmosis.
The anterior drawer test and varus-inversion tilt tests are useful clinical maneuvers employed to assess the severity of ankle sprain and ankle ligament integrity. Manipulating the foot beneath the tibia in the acutely sprained ankle may prove too painful, however, and is best reserved for the three-week follow-up visit.
An isolated ankle sprain can often be diagnosed without the use of a radiograph, but it is highly recommended that anteroposterior, lateral, and mortise x-rays of the involved ankle be obtained if there is any tenderness over the lateral malleolus, ankle joint, syndesmosis, or other bony structure. X-rays of the foot should be obtained if one has a high index of suspicion of fracture at the base of the fifth metatarsal, the calcaneal cuboid joint, or the lateral process of the talus.
Treatment
The goal of ankle sprain treatment is to prevent chronic pain, instability and disability. The first phase of routine ankle sprain treatment consists of rest, ice, compression, elevation, and usually the use of anti-inflammatory medications. An air stirrup brace and crutches can promote soft tissue healing and minimize atrophy of the calf musculature. For more severe sprains the use of a cast or fracture orthosis for two to three weeks is certainly acceptable. As the patient’s acute symptoms subside, weight bearing to tolerance with the use of crutches is recommended. Ice can be applied to the acute sprain, but any time during the first 48 hours after the injury contrast baths are most helpful to diminish swelling.
When a patient can weight bear without significant pain or swelling, usually two to four weeks after the acute injury, exercises to increase peroneal and active dorsiflexion strength are instituted. The patient should continue to use his air stirrup or brace so that the ligaments are not re-injured during this second phase of healing. Gentle stretching of the Achilles tendon is often also quite helpful. This phase of treatment, in which the dorsiflexors and evertors that normally prevent ankle ligament sprain are rehabilitated, is continued until the patient has full range of motion and normal strength.
Usually within four to six weeks after the acute ankle sprain, the patient can begin a program of functional conditioning with proprioception, agility and endurance training. Running in progressively smaller figures of eight is excellent for agility and peroneal strength. Using elastic bands for resisted eversion exercise is also helpful. The patient should not discontinue use of the ankle stirrup or return to athletic endeavors before he or she has full range of motion, full strength and no pain. Plantar flexion exercises and jumping should be avoided until these goals are met as they place the ankle in the position of least stability.
This treatment program may only take two weeks to complete for minor sprains or up to six or eight weeks for severe injuries. I will usually have my patients returning to competitive athletics use a functional brace or air stirrup for the entire next season of athletic competition to help prevent recurrent injury. This is especially important for soccer, volleyball and basketball players. There has never been proven scientifically, however, a role for preventive bracing in the athlete who has not sustained a prior ankle injury.
Potential pitfalls/referral decisions:
Serious injury is indicated by the presence of fractures of the foot and ankle, tears or subluxation of the peroneal tendons, a history of repeated giving way, stretch neuropraxia or other nerve injury, or failure to improve in six weeks with appropriate treatment.
Differential diagnosis:
The treatment regimen outlined above should prove effective for the vast majority of patients who sustain ankle sprains. The ankle sprain that won’t get better, however, is often due to concurrent injury. These injuries include fracture of the lateral process of the talus. Large, displaced, or intra-articular fractures of the lateral process of the talus require more active orthopaedic treatment. Simple, nondisplaced avulsion fractures, often found incidently on follow-up ankle x-rays, may not prove clinically significant. Avulsion fractures of the calcaneus, talus, lateral malleolus or base of the fifth metatarsal also indicate more serious injury.
Fracture of the proximal fibula associated with a rotational injury of the ankle within the distal mortise constitute the Maisonneuve fracture and almost always require surgical management.
Stretch neuropraxia of the superficial or deep peroneal nerve branches often leads to prolonged recovery, sometimes requiring six to twelve months for resolution of symptoms.
One of the more commonly missed diagnoses after ankle sprain presenting to my office includes osteochondral fracture of the talar dome. This can easily be missed even on high quality initial radiographs and often requires MRI or CAT scan for confirmation.
Peroneal tendon tear or subluxation is often a difficult diagnosis to make unless one is specifically looking for this pathology. These patient’s have persistent swelling posterior and sometimes straight lateral to the lateral malleolus. There is a popping or crepitant sensation reported by the patient and they have a greater difficulty descending stairs and walking on uneven ground than a patient with a routine ankle sprain. Often the peroneal tendon can manually be reduced and its finding anterior and lateral to the lateral malleolus is quite dramatic and diagnostic.
Also associated with the ankle sprain that won’t get better is a subtalar joint sprain. The patients who have subtalar pathology often have worse pain and instability on uneven ground than while walking on level surfaces. These patients often report that even a small pebble or stone on an otherwise level path can cause their “ankle” to give way. Most simple subtalar joint sprains will improve with the three-phase ankle ligament treatment protocol outlined above.
Injury to the syndesmosis, the thick ligaments connecting the distal tibia and fibula, occurs in approximately five percent of all ankle sprain. This injury is often referred to as a “high” ankle sprain. Recovery time from this injury is greatly increased compared to that of a simple “lower” ankle sprain. Sometimes late reconstruction of the syndesmotic ligament with passage of a transverse screw from the fibula into the distal tibia is required.
Adverse outcomes of treatment and injury:
Casting and ankle immobilization for more than three weeks may cause leg muscle atrophy, joint stiffness, and a slower return to sports or work. Therefore, casting should be reserved for only the most severe cases and consideration of functional immobilization with an air stirrup may be more appropriate. Oral anti-inflammatory agents may cause renal, hepatic or gastric complications.
An undetected ankle or foot fracture may have serious consequences. There may be chronic pain following a severe sprain even without the presence of a fracture. Severe sprains may also result in chronic instability and the possibility of arthritis. Chronic instability is usually secondary to incomplete rehabilitation and may occur in up to 40 percent of all ankles sprains.
Summary
While ankle sprains are very common injuries seen by orthopaedists and the general practitioner alike, appropriate three-phase functional rehabilitation can provide excellent results with a minimum of comorbidities and adverse outcomes. If the physician keeps in mind the differential diagnosis outlined here, treatment can be tailored to the patients needs and complete recovery expedited.
References
- American Academy of Orthopaedic Surgeons. Position statement on the role of preventive rehabilative and functional bracing. www.aaos.org.
- Snider, Robert K., editor. Essentials in musculoskeletal care, American Academy of Orthopaedic Surgeons, American Academy of Pediatrics. Pages 390 – 393, 1997.
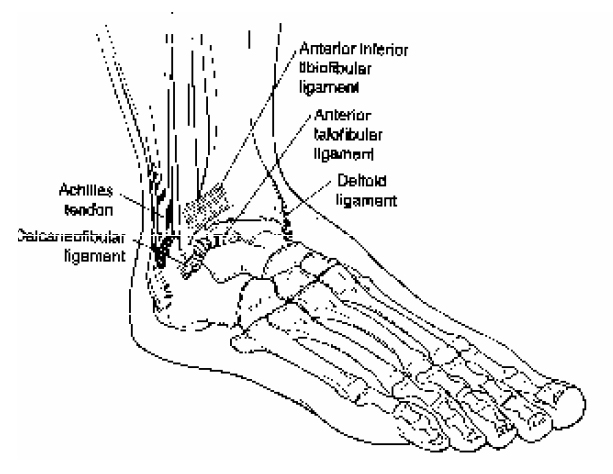 Figure 1. Ligaments of the ankle.
Figure 1. Ligaments of the ankle.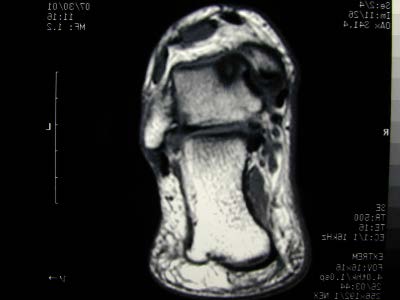 Figure 2. MRI of ankle of 32-year-old male presenting nine months after acute ankle “sprain”. MRI is consistent with osteochondritis dissecans lesion of medial talar dome with surrounding bone marrow edema.
Figure 2. MRI of ankle of 32-year-old male presenting nine months after acute ankle “sprain”. MRI is consistent with osteochondritis dissecans lesion of medial talar dome with surrounding bone marrow edema.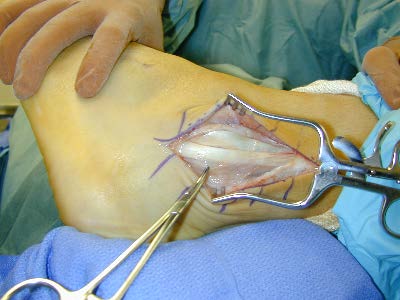 Figure 3a. Intra-operative appearance of completely dislocated peroneus brevis and longus tendons after traumatic ankle “sprain”.
Figure 3a. Intra-operative appearance of completely dislocated peroneus brevis and longus tendons after traumatic ankle “sprain”. Figure 3b. Intra-operative appearance of same patient after peroneal retinacular ligament reconstruction and fibular osteotomy with internal fixation. Note the peroneal tendons are now behind the lateral malleolus and placed deep to the calcaneal fibular ligament.
Figure 3b. Intra-operative appearance of same patient after peroneal retinacular ligament reconstruction and fibular osteotomy with internal fixation. Note the peroneal tendons are now behind the lateral malleolus and placed deep to the calcaneal fibular ligament.


 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.