Robotic Total Knee Replacement
Apr 14, 2022R. Alex Sweet II, MD
My experience since performing the first Robotic Total Knee Replacement In Baptist Health History
History of Total Knee Replacement

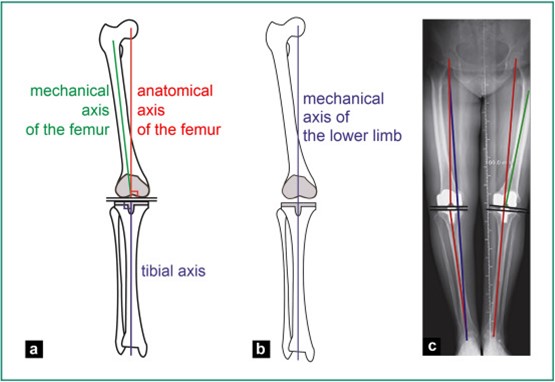
The first “Total Knee” was implanted in 1968. With inferior mechanics, materials and design, these were fraught with problems and early failure was common. Early alignment was measured using rods inserted into the femur (thigh bone) and down the tibia (shin bone). This allowed surgeons to estimate the amount of bone to be removed and the proper alignment for the bony cuts. These estimations used average values calculated from cadaver studies that led to an “average alignment axis.” This average alignment was then used for all patients and even today remains the standard for total knee surgery. With improvements in materials and engineering, outcomes have greatly improved, but there remains a great degree of error.
The Problems

 Unfortunately about 20% of total knee replacement patients are “not satisfied”. This has been shown in countless orthopedic studies published starting in the 1980s and is still shown to hold true with modern techniques today. While these patients may not have bad outcomes, there is plenty of room for improvement. People with curved femur or tibia bones, or with anatomy a degree or two different than the “average” can drastically change the performance of the knee. Even if by chance the alignment is perfectly measured, modern saws used to cut the bone have been shown to have up to a 2 degree error, leading to inaccuracy and potentially poor outcomes.
Unfortunately about 20% of total knee replacement patients are “not satisfied”. This has been shown in countless orthopedic studies published starting in the 1980s and is still shown to hold true with modern techniques today. While these patients may not have bad outcomes, there is plenty of room for improvement. People with curved femur or tibia bones, or with anatomy a degree or two different than the “average” can drastically change the performance of the knee. Even if by chance the alignment is perfectly measured, modern saws used to cut the bone have been shown to have up to a 2 degree error, leading to inaccuracy and potentially poor outcomes.
Modern Solutions
There have been countless advancements in total knee surgery over the decades. Knee replacement surgeries centered around preoperative imaging with a CT or MRI scan, called “patient specific”, create personalized cutting jigs for each patient. Unfortunately these have done nothing to improve outcomes and patients are required to pay the cost of the CT/MRI. Even modern total knee designs such as the Journey II have made incredible advancements in design and materials. However a portion of these patients still remain unsatisfied.
Robotic TKA
How it Works:
- MAPPING: A probe is used to mark out all relevant anatomic locations in the knee and even the ankle (no incision at the ankle required). Markers are placed on the leg that record 3-D positioning. The knee and hip are then taken through motion. The computer recognizes the entire bony axis of the leg without any estimation or deviation. The tension of the soft tissue can also be measured.

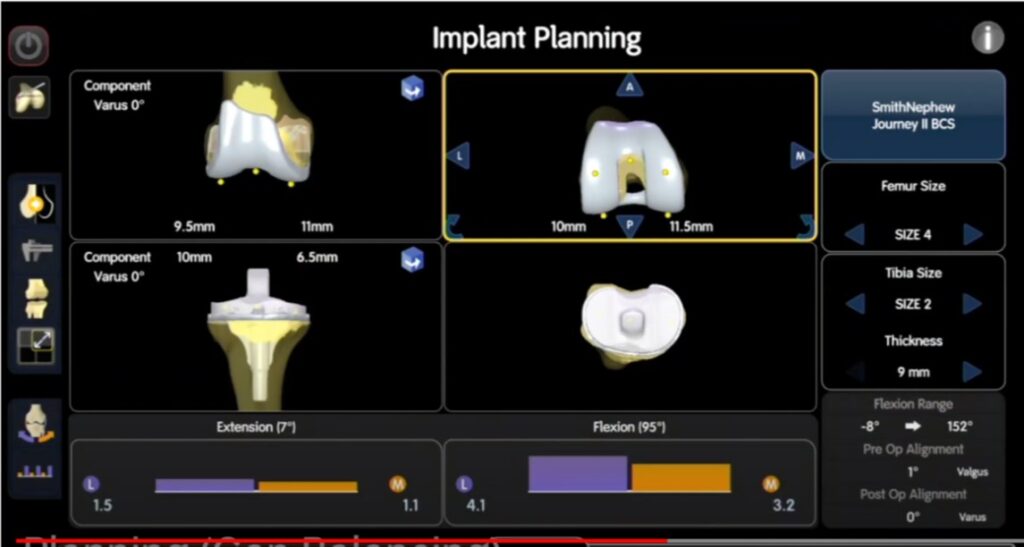
2. PLANNING: The knee replacement can be planned to the exact fraction of a degree to allow for full range of motion with perfect alignment and stability. The bony cuts are determined and the size of the knee replacement parts can be measured. This can all be done in a matter of seconds using the computing power of the robot. However it still allows for surgeon discretion to design the knee for the patients’ specific needs and desired outcomes. This ensures ACCURACY.
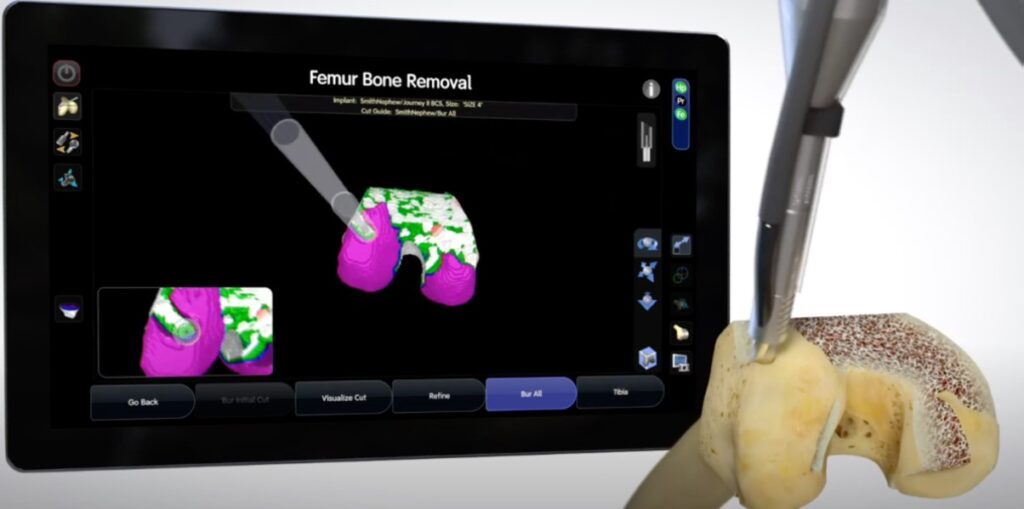
3. BONE CUTS: Next the femur and tibia bones are resected. Previously, this was done using an inaccurate saw, but now a burr (wirelessly connected to the computer) does the resection. The robot knows exactly what bone needs to be resected and only turns on the burr when needed. Once the planned amount of bone has been resected, or if the surgeon gets too close to a ligament or soft tissue, the burr automatically shuts off. It will not allow deviation from the plan in step 2. This ensures PRECISION.
4. VERIFICATION: At any time during the surgery the surgeon can utilize the robot to ensure everything is going to plan and changes can be made if necessary.
Improved Outcomes:
 There is no training, education, course, or amount of experience that allows a surgeon to be as precise or accurate as a robot. When you combine the expertise and judgement of a well-trained surgeon with the advantages of a robot, the outcome is astounding. For the first time since the 1970s we have the technology to improve upon surgical outcomes and performance of total knee replacement.
There is no training, education, course, or amount of experience that allows a surgeon to be as precise or accurate as a robot. When you combine the expertise and judgement of a well-trained surgeon with the advantages of a robot, the outcome is astounding. For the first time since the 1970s we have the technology to improve upon surgical outcomes and performance of total knee replacement.



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.