Reconstruction of Multiplanar Ankle and Hindfoot Deformity with Intramedullary Techniques
Aug 21, 2019George Edward Quill, M.D. (Retired 2023)
ABSTACT:
The goal of ankle and hindfoot reconstruction should always be to address the presenting concerns of the patient and the deformity, as well as to achieve a stable, functional and plantigrade foot. These goals are accomplished by appropriate preoperative patient assessment and planning, as well as by employing meticulous intraoperative technique and aftercare. An algorithmic approach to multiplanar hindfoot deformity is presented in this article along with the author’s preferred method of treatment, aftercare and management of complications. Great emphasis is given to preoperative planning in order to ensure the best possible postoperative outcomes.
INTRODUCTION:
Disabling ankle and hindfoot deformity presents in myriad forms and may be associated with various neuromuscular deficits, as well as functional limitations that can be quite painful (2,11,29,29). Multiplanar ankle and hindfoot deformity may result from primary osteoarthritis or rheumatoid arthritis, as well as the sequelae of significant open or closed trauma (21, 32). Skeletal defects after tumor resection, failed prior reconstructive arthrodesis or arthroplasty techniques, as well as the sequelae of poliomyelitis, paraplegia and hereditary sensorimotor deficits can provide challenges to the treating orthopaedic surgeon (24,33,34). The goal of treatment should always to be to address the presenting concerns of the patient and the deformity, as well as to achieve a stable, functional and hopefully pain-free plantigrade foot. These goals are accomplished by appropriate preoperative assessment of the patient and radiographic studies and meticulous preoperative planning with detailed attention to intraoperative surgical technique. Diligent aftercare and aggressive management of complications will ensure the most optimal postoperative outcome.
PATIENT INTERVIEW:
One of the most telling and helpful questions a surgeon may ask his patient is, “if you could point with one finger to the area that bothers you the worst, what would you show me?” Localized pain is often mechanical or arthritic in etiology and is the type we can most successfully address. Generalized pain, neuritic pain, vascular insufficiency or neuropathic pain is difficult to improve with an operation. A good history is imperative in setting us on the path to the correct treatment and often will elucidate whether the problem at hand was due to antecedent trauma, either open or closed injury, or whether primary arthritis is a concern. It is important to ascertain whether the patient’s pain is present at rest or activity related; whether there is radiation distally or proximally to this discomfort, and how it may impart upon gait pattern or the ipsilateral knee, hip or back. When pain is worse on uneven ground than it is on level surfaces the etiology of the pain is often due to the subtalar joint or slightly less commonly the transverse tarsal joints (31). The history of giving way is often present in a patient with an unstable ankle or fixed hindfoot varus, which also may be associated with peroneal insufficiency and weakness of eversion power (Figure 1). A history of locking usually indicates the presence of an intra-articular loose body.

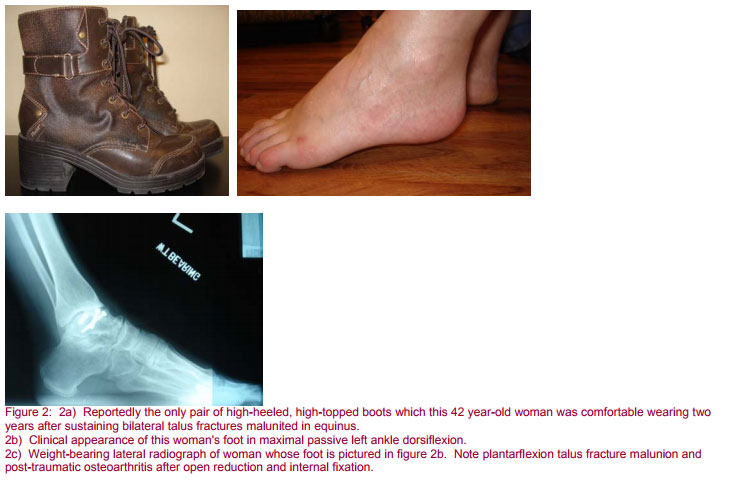
Shoewear limitations may be present and one should ascertain whether the patient perceives an abnormal shoewear pattern. Determining the prior use and benefit, if any, from bracing, injections, and oral medications will help guide future treatment. Patients may also have proximal deformity that requires reconstruction. In order to ensure that the foot is positioned properly in space and in a plantigrade posture relative to the floor any proximal realignment osteotomy or total knee arthroplasty should be performed prior to any ankle or hindfoot reconstruction.
Secondary to the potentially long postoperative recovery, it is important to ascertain whether the patient has help at home and whether the physical layout of their home is conducive to postoperative mobility. Consider the use of a scooter or wheelchair if the patient does not have the upper extremity strength to use crutches or a walker. Preoperative assessment with a physical therapist will objectively determine the patient’s ability to use an assistive device.
PATIENT EXAMINATION:
A thorough musculoskeletal, neurologic, and vascular examination of the patient is critical. The surgeon must evaluate both lower extremities, the gait pattern and the biomechanical axis of the involved limb. In addition to a careful musculoskeletal and neurologic exam, one should assess the location of calluses, ulcerations, scars and soft-tissue defects. Assessment of the wear pattern of the patient’s current footwear can help determine subtle malalignment of the hindfoot.
As an example, the patient with a tendency to genu recurvatum in stance secondary to an equinus contracture or anterior tibiotalar abutment with discrete calluses on the plantar forefoot would most likely be comfortable in a higher heeled shoe to minimize the stress on the knee and place the ankle in the patient’s functional range of motion. (Figure 2).
A patient with Charcot-Marie-Tooth disease will typically have a varus hindfoot, peroneal muscle insufficiency and often a plantar flexed first ray with a callous under the first metatarsal head (2, 3, 15). The patient with severe hindfoot valgus will have subfibular impingement, deltoid and posterior tibial tendon insufficiency and fixed forefoot varus that must be taken into account when using intramedullary fixation for reconstruction (29, 30). If the forefoot deformities are passively correctable then it may be possible to achieve a plantigrade foot without performing forefoot osteotomies or extending a hindfoot fusion mass to the midfoot in the form of an extended pantalar arthrodesis (32).
PREOPERATIVE ASSESSMENT INCLUDING RADIOGRAPHS AND ADDITIONAL DIAGNOSTIC TESTING:
At a minimum, weight bearing AP x-rays of the ankle as well as AP and lateral x-rays of the involved foot while standing should be obtained. These films should include as much of the distal tibia as necessary to visualize any existing hardware, malunited fractures or other potential stress risers that may be present (Figure 3).
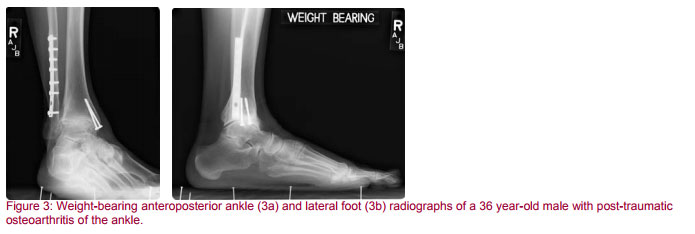
Additional special views, such as oblique or Harris-Beath views of the foot to assess for tarsal coalition may be necessary. It is often helpful to obtain comparison x-rays of the contralateral uninvolved limb for preoperative purposes (31). Often we will x-ray the knee joint above the hindfoot to be reconstructed to assess for coronal plane abnormalities. We have also found it helpful to get tangential views of the sesamoid on special occasions when assessing potential etiologies of forefoot discomfort because the sesamoids may be arthritic, fractured or unduly proud if subluxed. Stress radiographs are helpful in elucidating ankle or syndesmotic instability.
Diagnostic and therapeutic injections of local anesthetic can be very helpful to differentiate the anatomic source of pain (28,30). For example, in a patient with lateral hindfoot pain, an injection in the sinus tarsi can distinguish between pains arising from pathologic peroneal tendons versus that attributable to an arthritic subtalar joint.
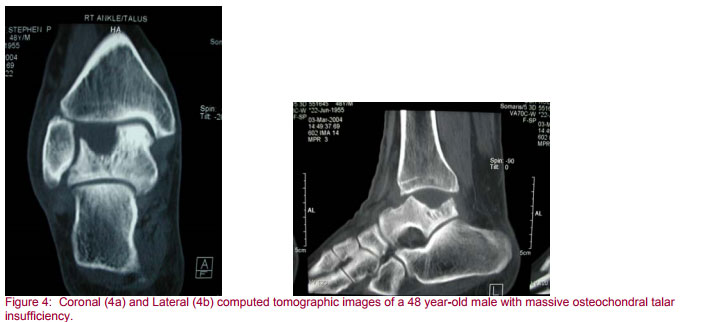
Computed tomography with both feet and ankles in the gantry at the same time is a useful preoperative tool in evaluating cases with suspected subtalar pathology, bone loss, neoplasia infection, or trauma (Figure 4).
Magnetic resonance imaging helps greatly in ascertaining the presence or absence of bone marrow edema, soft tissue pathology, synovial proliferation, and tibiotalar avascular necrosis. Technetium nuclear medicine bone scans are sensitive tests that will be positive in any etiology that increases circulation to bone. Technetium and indium labeled white blood cell scans can be useful in planning surgery for the indication of osteomyelitis (9).
PREOPERATIVE PLANNING:
A good place to start the preoperative planning is in assessing the apex of the clinical deformity. The surgeon must assess the direction of the apex of the deformity. In cases of rotational or axial hindfoot malalignment the foot may be at a normal angle to the longitudinal axis of the limb. In cases of severe varus or valgus, the deformity is more obvious. When assessing the deformity the surgeon must ascertain what needs to be done to establish a plantigrade foot. The treatment for a fixed, sensate and empowered limb is very different from that for a flexible, insensate or flail foot.
Preoperatively the surgeon must determine whether there is normal neuromuscular function about the foot and ankle. Are the posterior tibial tendon and peroneal muscles and tendons functioning? Does the patient have a drop foot, persistence of a congenital or developmental deformity, or even a hereditary sensorimotor neuropathy or the sequelae of poliomyelitis?
Another very important clinical question is whether the subtalar joint can be spared, especially when the surgeon is contemplating the use of intramedullary fixation for hindfoot reconstruction.
Preoperatively the surgeon must also ensure that he has available the appropriate instrumentation and personnel, as well as intraoperative fluoroscopic imaging. The anesthetic technique should be carefully considered, as should positioning of the patient on the operating room table.
Lastly the surgeon will want to consider adjuvants for healing, including bone graft that may be autograft, allograft or synthetic. One may consider either external or implanted electrical bone stimulation to improve healing rates. In this day and age one must strongly consider employing available orthobiologic adjuvants as well for optimal healing. The surgeon may choose from platelet-derived autologous growth factors, bone marrow aspirate, demineralized bone matrix and even bone morphogenetic protein. All of the factors mentioned in this section are carefully considered preoperatively and impact the operative technique to be discussed in the next section. Specifically, the surgeon must consider preoperatively the advantages, disadvantages, indications and contraindications of intramedullary fixation techniques in reconstructing ankle and hindfoot deformity.
The advantages of medullary nail fixation for ankle and hindfoot reconstruction include the fact that intramedullary nails are load-sharing devices especially useful in the treatment of the osteopenic patient and that they provide excellent early stability, ensuring position and alignment from the very start(17, 32). Medullary nail fixation devices are also advantageous compared to more traditional methods of fixation because often a shorter period of postoperative immobilization and activity restriction is required (15, 25, 33). Intramedullary fixation is very advantageous for the neuroarthropathic patient or one who has insufficiency of the distal tibia, talus or calcaneus (7, 24).
Medullary nail fixation is indicated for arthrodesis where there has been avascular necrosis of the talus, failed ankle replacement with subtalar intrusion, or a failed ankle fusion with insufficient talar body (5, 6, 10, 13, 14, 19, 24, 35). Other indications include primary or secondary osteoarthrosis, rheumatoid arthritis, the sequelae of trauma (especially distal tibial pilon fractures) and for management of patients with neuromuscular disease, pseudarthrosis, neuroarthropathy or skeletal defects after tumor resection (2-4, 7, 8, 11, 15, 17, 21, 24, 27-30, 32, 33, 36-41).
Medullary nail contraindications include the dysvascular extremity or one in which there is a severe active infection (9). Relative contraindications to medullary nail fixation include the patient with insufficient plantar padding as most of these devices are inserted in retrograde fashion through the heel. The surgeon would also think twice about passing a medullary nail across an otherwise normal subtalar joint except in the cases where it is worth while to fuse the subtalar joint and the ankle at the same operative procedure due to avascular necrosis of the talus, talar insufficiency, or distal tibial insufficiency due to prior trauma or tumor resection. In these cases it would be acceptable to fuse an otherwise normal subtalar joint in order to span the diseased more proximal bone with an intramedullary fixation device. Even severe, fixed angular deformities of the distal tibia, ankle and hindfoot can be overcome with periarticular osteotomies that make a collinear reduction of the tibia, ankle and hindfoot possible in order to pass a retrograde intramedullary nail (30, 32).
INTRAOPERATIVE TECHNIQUE: AUTHOR’S PREFERRED METHODS:
The general principles of intramedullary fixation for hindfoot and ankle reconstruction are as follows. The surgeon’s goal should be to achieve a plantigrade foot while relieving pain, correcting deformity and producing a solid fusion. A plantigrade foot is defined as one which is held at approximately 90 degrees to the long axis of the tibia and in no more than 5 to 7 degrees of hindfoot valgus. In stance, a plantigrade foot is one in which a tripod of weight bearing, including the heel, as well as the first and fifth metatarsal heads, is achieved simultaneously (16, 22, 26).
The first and fifth metatarsal heads must strike the ground together in stance. Equinus leads to genu recurvatum and early heel off. The patient with an equinus malunion will walk with external rotation of the hip (Figure 5). Dorsiflexion is better tolerated than plantar flexion if it is minimal. Too much dorsiflexion at the ankle results in a painful, uncomfortable heel strike and unsatisfactory push-off power. In determining ankle dorsiflexion during hindfoot and ankle reconstruction with medullary fixation, the surgeon must also take into account forefoot equinus (Figure 6) (23).

Gellman, et al., determined the deficits after ankle fusion alone were 51 percent and 70 percent respectively for dorsiflexion and plantar flexion. Deficits in dorsiflexion and plantar flexion are 53 percent and 71 percent respectively after tibiotalocalcaneal fusion and were not significantly different from the deficits after ankle fusion alone. These authors found that inversion and eversion, however, were 40 percent less after tibiotalocalcaneal fusion than after ankle fusion alone. Deficits after pantalar arthrodesis were quite significant. In dorsiflexion and plantar flexion these were 63 and 82 percent respectively. Inversion and eversion were 72 and 67 percent respectively less after pantalar arthrodesis then they were after ankle fusion alone (12).
The patient’s longitudinal biomechanical axis must be such that weight bearing forces are carried directly through the center of the hip, knee and ankle. It is normal that the heel be in approximately 5 degrees of valgus and thus to the lateral side of that line (20, 31).
Another general principle is that the surgeon should fuse all painful and/or arthritic joints, but use joint sparing procedures such as cheilectomy and periarticular realignment osteotomies whenever possible. When the surgeon does perform arthrodesis, the fusion should be fixed as rigidly as possible, bone grafted liberally, and protected postoperatively.
Bony prominences should either be resected or osteotomized off the plantar weight bearing aspect of the foot. Hardware and bone prominences should not be left in subcutaneous places of prominence such as the retrocalcaneum.
The surgeon should avoid the formation of painful scars and neuromas, transposing the latter whenever they are encountered. In short, the surgeon should use a no-touch technique and be gentle with the soft tissues. Fascia and dermal tissues should be closed well so that the skin edges may be apposed and everted without tension at the end of the case. Along these lines, the surgeon should also preserve the plantar padding and stage procedures on different days when the magnitude of the deformity necessitates. For example, a patient with pantalar arthritis might better be served with a healthy, well-aligned triple arthrodesis of the hindfoot and a total ankle replacement above it than he would a pantalar fusion employing intramedullary fixation devices (34).
Intramedullary nailing has proved to be a solid method of fixation for achieving ankle and hindfoot arthrodesis (4, 6, 25). A nail inserted through the plantar aspect of the foot can afford excellent stability, position and alignment. The process of ankle and hindfoot arthrodesis, often called tibiotalocalcaneal arthrodesis, using an intramedullary nail, usually involves an ankle arthrotomy, preparation of the joint surfaces, and then placement of the nail through a plantar incision. Screws are placed proximally through the tibia and the nail in a standard fashion and, after compression across the fusion sites, the nail can be mechanically locked distally with screws into the calcaneus and talus (32).
In a patient with severe external rotational deformity of the foot on the leg or for the one who has severe preoperative valgus deformity with the apex directed medially, the author usually positions the patient supine on the operating room table. The foot is positioned with the heel very close to the end of a radiolucent operating room table with C-arm intraoperative fluoroscopic imaging available. A note is made of the anatomy of the contralateral uninvolved lower extremity and the mechanical axis of the index extremity. Most patients will have adequate external rotation and internal rotation at the hip to allow anteroposterior and lateral imaging of the foot intraoperatively with the fluoroscope. For medullary nail fixation devices that allow for multiplanar locking screws to be inserted, even the supine patient, given enough flexion and rotation at the hip, can be managed appropriately in this fashion. General or regional anesthesia is employed. Regional blocks for postoperative pain relief are used on a regular basis in the author’s practice. Parenteral antibiotics are given on a prophylactic basis preoperatively. Landmarks are noted and the skin incision is designed to minimize soft tissue trauma and stripping.
Under thigh tourniquet hemostatic control a longitudinal incision is usually made over the apex of the deformity medially in a patient with preoperative valgus. Dissection is carried sharply through the dermis and blunt dissection used deep to that exposing the medial malleolus in this approach. Care is taken to note and protect the course of the posterior tibial tendon as well as the posteromedial neurovascular bundle.
The patient with severe preoperative valgus will generally undergo a medial malleolar osteotomy to include a varus producing, medially based closing wedge osteotomy through the tibiotalar fusion site (Figure 7). If the subtalar joint is in severe valgus as well, a small sinus tarsi incision can be made to approach the subtalar joint from the lateral side translating it medially and leaving it such that the calcaneus lines in collinear fashion with the talus and tibia. Alternatively, a careful medial approach to the subtalar joint can be made just dorsal to the posterior tibial tendon and posteromedial to the neurovascular bundle. This medial approach in patients presenting with severe preoperative valgus will obviate the potential problem of closing under tension a lateral wound once the valgus has been corrected.

Chisel, curette and rongeur are used to denude diseased articular cartilage. Multiple fenestrations are made with a small-diameter drill bit on either side of the arthrodesis site to perforate hard subchondral bone, and encourage bleeding and bony ingrowth. Once a collinear reduction of the tibia, talus and calcaneus is achieved, a small plantar incision is made longitudinally anterior to the subcalcaneal fat pad. Sharp dissection is carried through the dermis with blunt dissection taken deep to that. A blunt key elevator is used to sweep away the intrinsic muscles and neurovascular structures on the plantar aspect of the foot. In this fashion, blunt dissection can be taken all the way down to the inferior surface of the calcaneus. The ideal staring point for the insertion of a guidewire is approximately 2 centimeters proximal to the calcaneal cuboid joint and lateral to the sustentaculum tali.
In this fashion a guidewire is passed through the inferior cortex of the calcaneus, across the subtalar and ankle fusion sites and into the distal tibia. Its position is ascertained on both the AP and lateral projections of the C-arm fluoroscopic image and overdrilled with a cannulated drill bit measuring approximately 7 millimeters in diameter.
The drill and its guidewire are removed and, next, a bulb-tipped guidewire is passed in retrograde fashion through the calcaneus, talus and into the medullary canal of the distal tibia.
A series of progressively larger flexible reamers are passed over this bulb-tipped guidewire to prepare the tibiotalocalcaneal canal for the nail. We usually start with an end-cutting reamer of about 8 millimeters in diameter then ream in half-millimeter increments up to 0.5 to 1.0 millimeters larger than the intended outside diameter of the nail to be used for fixation. A more aggressive advance in the width of the reamers can result in incarceration of the reamer within the tibia.
The length of the nail chosen should be such that its proximal tip does not end at the distal metadiaphyseal tibial isthmus. Overzealous reaming here or the presence of a titanium medullary nail can cause a potential stress riser leading to cortical stress hypertrophy and insufficiency fractures. Ideally a 15 to 18 centimeter nail can be inserted in retrograde fashion and end either distal or just proximal to this isthmus. In the neuropathic patient nails as long as 270 to 300 millimeters have been used to provide better stability and off-load stresses of the neuroarthropathic hindfoot.
As a general rule, it is critical to span skeletal defects including those left by removal of hardware placed at prior procedures by at least one and one half to two tibial diameters. Failure to do so will result in a stress riser and potential fracture through the defect.
The distal end of the nail should be countersunk or flush with the inferior cortex of the calcaneus. Most manufacturer’s nails include the capability of compression across the ankle and subtalar fusion sites and the surgeon will usually do best to countersink the nail into the hindfoot to the depth he anticipates he will compress across the fusion sites to prevent prominence. The nail is locked proximally in the tibia with at least two locking screws that can be targeted with extramedullary aiming devices or freehanded for the longer, more proximal nails.
It is advantageous to add bone graft across the fusion sites prior to inserting the nail and compressing the arthrodesis site. Compression across the ankle fusion site is often improved by osteotomizing the lateral malleolus if the fibula is intact. At this point it is imperative to check the rotation of the limb before locking distally. Ideally, the ankle should be in 0 degrees of dorsiflexion, no more than 5 to 7 degrees of hindfoot valgus, and should have external rotation either symmetric with the contralateral uninvolved side or in a position at which the second ray of the foot lines up with the anteromedial tibial crest of the involved leg.
The nail is then locked distally in the talus and calcaneus (Figure 8). I have found it advantageous to have a nail with multiplanar locking choices. Bench studies have documented as much as forty percent increase in torsional rigidity when locking screws are placed at orthogonal angles (32). Furthermore, recent advances in medullary nail techniques include targeting slots for placement of tangential fixation screws from the calcaneus into the distal tibia. This use of a screw spanning the subtalar and tibiotalar joints can greatly increase the torsional rigidity of the construct and augments the fixation in the talus and calcaneus (30). Often when one addresses the preoperative valgus deformity such as described here it is impossible to lock distally from medial to lateral without putting at risk the medial neurovascular structures. If this is the case, lateral to medial and posterior to anterior locking screws are employed for distal fixation. Further bone grafting is done and, if indicated, implanted bone stimulation devices inserted. I have found it helpful to add demineralized bone matrix putty at the fusion sites to increase healing rates and help with hemostasis. An end cap is placed in the nail after its targeting device is removed in order to restrict medullary blood flow and protect the threads of the nail in the event its removal may be required in the future. Most nails are not inserted with the intention of removal and may be left in place indefinitely.

Locking screw heads are countersunk wherever possible so they are not prominent subcutaneously. The wound is usually closed over a closed suction drainage tube and a bulky dressing incorporating posterior and coaptation plaster splints applied with gentle Ace wrap compression over padding. The drain is placed to suction and the patient is brought to the recovery area after checking circulatory status, position and alignment. Permanent radiographs are quite helpful and plantigrade reduction must be confirmed on the table before the patient’s anesthesia is reversed. The surgeon must ensure satisfactory alignment, reduction, position and fixation before terminating the case.
The patient with preoperative varus deformity and/or instability and weakness is positioned in the lateral decubitus position with the effected side up. Again a radiolucent operating room table is used and an axillary roll is used in the recumbent axilla. Great care is taken to pad all bony prominences and the patient is fastened to the table with the contralateral limb flexed at the hip and knee so as to be out of the way for fluoroscopic imaging. Again the patient with good external rotation at the hip will be afforded appropriate fluoroscopic imaging without having to rotate the C-arm.
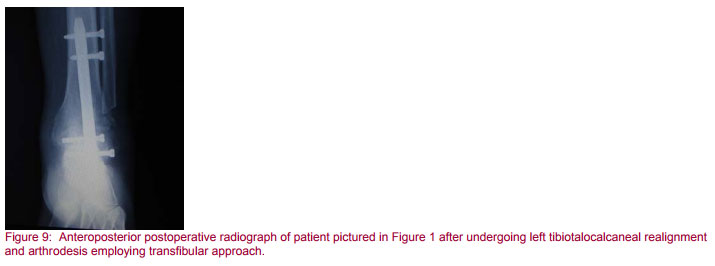
For the patient with severe preoperative varus I would choose the transfibular approach affording excellent exposure for ankle and subtalar fusion (Figure 1) (1, 18, 21, 28, 32). The patient’s own fibula also serves as a wonderful source of autogenous bone graft material. The patient undergoing medullary fixation for this type of preoperative deformity will also have better shoe fit without impingement of a prominent fibula using the transfibular approach.
A longitudinal incision is made over the posterior fibula, which then curves anteriorly at its distal tip along the peroneal tendons. Care is taken to note the course of the existing neurovascular structures and tendons. The distal 4 to 5 centimeters of fibula is resected in a beveled fashion at a level approximately 2 centimeters proximal to the tibiotalar joint line. This will normally preserve the distal tibiofibular syndesmosis and postoperatively this will prevent fibular instability (Figure 9). Alternatively, the distal fibula can be skeletonized, osteotomized and later re-fixated with screws to the tibia and talus to add to the fusion mass (4).
The peroneal tendons are preserved as is the thick periosteal envelope from which the fibula was harvested. This is saved to be used as a discreet anatomic layer for closure at the end of the case. An incision is extended distally to the sinus tarsi to allow subtalar joint visualization. Ankle and subtalar joint preparation are crucial to successful fusion and the author uses chisels, curettes and rongeurs and multiple holes for fenestration as outlined previously.
The tibiotalar joint can be denuded of cartilage in a congruent fashion thus preserving the normal distal tibial concavity and talar dome convexity. In this fashion external rotation positioning is easier to ascertain.
Alternatively, a transverse saw cut can be made across the distal tibia and the dome of the talus bringing the ankle into neutral position as the matching talar cut is performed (28). The posterior and lateral talar surfaces are decorticated to allow for greater fusion surface, as is the articular surface of the medial malleolus denuded of diseased cartilage. Again, the best position for arthrodesis is neutral dorsiflexion and approximately 5 degrees of hindfoot valgus with external rotation symmetric with contralateral uninvolved extremity. Appropriate external rotation is achieved when the anteromedial crest of the tibia lies parallel with the second ray of the involved foot (16, 23).
Following preparation of the bony surfaces, a 2 to 3 centimeter longitudinal plantar incision is made anterior to the subcalcaneal fat pad as described previously.
The ideal position for the plantar calcaneal entry site is well anterior to the weight bearing surface of the calcaneal tuberosity and approximately 2 centimeters posterior to the articulation of the calcaneus with the transverse tarsal joints. In the coronal plane, the entry site should line up with the center of the tibial medullary canal. Guide wires and flexible reamers are used to prepare the tibiotalocalcaneal canal as mentioned previously (33).
Once inserted, the proximal end of the nail should extend at least one and a half to two tibial diameters above any potential cortical stress risers. This would include nonunion sites, tibial fractures, osteotomies sites, or cortical holes that may exist after previous hardware removal. Ideally the nail should be countersunk 5 to 10 millimeters in the plantar cortex of the calcaneus. In certain cases of tibiocalcaneal fusion it is not unusual to have the distal portion of the nail extend 5 to 10 millimeters distal to the inferior cortex of the calcaneus and still have a sufficient plantar pad for pain free weight bearing postoperatively. The remainder of the outrigger assembly targeting nail insertion and locking with compression across the fusion sites is as describe previously (32).
The techniques just described will appropriately address the vast majority of patients presenting with deformities ranging from the extremes of varus to valgus hindfoot malalignment in the coronal plane and any axial malalignment in the transverse plane. The patients thus described would prove to be excellent candidates for tibiotalocalcaneal arthrodesis. Patients for whom there is fixed deformity including and distal to the transverse joints, however, will have to be considered for additional surgical procedures.
As mentioned previously in this chapter, it is imperative that the forefoot be plantigrade in such a fashion that the first and fifth metatarsals head strike the ground with weight bearing at the same time.
The patient with severe preoperative pes planovalgus and a fixed forefoot varus will either require derotational osteotomies through the transverse tarsal joints to a plantigrade posture and extension of the fusion mass to include a pantalar arthrodesis with medullary nail fixation (Figure 8) or, if the transverse tarsal joints are not arthritic, a plantar flexion opening wedge osteotomy at the base of the first metatarsal or through the medial cuneiform may be performed. In this fashion, the patient’s first and fifth metatarsals head strike the ground appropriately (29,30,32).
The patient with preoperative pes cavovarus and fixed forefoot valgus presents the opposite problem and will have a hyper plantarflexed first ray requiring either pantalar arthrodesis or, if the transverse tarsal joints are to be preserved, a dorsiflexion osteotomy at the base of the first metatarsal in order to achieve a plantigrade posture (29, 30, 32, 41).
As mentioned previously, fixed forefoot equinus, as often happens in the patient with pes cavus, must be taken into account when determining the appropriate position of hindfoot and ankle fusion with medullary fixation devices. Even though the ankle may seem as if it is at neutral dorsiflexion relative to the long axis of the tibia, if the surgeon does not account for the fixed preoperative forefoot equinus, the patient will still walk postoperatively with a back-kneed, recurvatum type gait (12). In order to preserve midfoot and forefoot mobility when addressing such patients, I will often perform an anterior, closing wedge dorsiflexion osteotomy through the tibiotalar fusion site before fixing it with a medullary fixation device to ensure a plantigrade posture postoperatively (Figure 2).
AFTERCARE:
In the author’s personal series of employing medullary fixation for hindfoot and ankle reconstruction, more than 95 percent union rate occurred within twelve to fourteen weeks after surgery for patients undergoing the index fusion for diagnoses of osteoarthritis or rheumatoid arthritis. I prefer the patient be immobilized in a nonweight bearing, short-leg cast for the first six weeks followed by weight bearing to tolerance in a walking cast for an additional six weeks. Often transition to regular shoes is aided by the use of a removable fracture orthosis that includes a rocker bottom. I prefer to immobilize the neuropathic patients at least four weeks longer than the twelve week routine just mentioned. Radiographs are obtained intraoperatively with suture removal two weeks postoperatively, and every four weeks until union. Radiographs are obtained in the AP and lateral projection on a cassette long enough to include the entire length of a medullary nail.
SUMMARY:
Medullary nail fixation for reconstruction of multi planar, ankle and hindfoot deformities has proven a safe, effective and reliable method of fixation. The best results in achieving arthrodesis with this method are achieved for patients undergoing their index reconstruction procedure for a diagnosis of primary osteoarthritis or rheumatoid arthritis. Close attention to preoperative planning and intraoperative detail will ensure the best possible outcomes with fewest complications.
- Adams JC: Arthrodesis of the ankle joint: experiences with the transfibular approach. J Bone Joint Surg 1948; 308:506-511.
- Ansart MB: Pan-arthrodesis for paralytic flail foot. J Bone Joint Surg1951; 503-507.
- Barrett GR, Meyer LC, Bray EW, et al: Pantalar arthrodesis: a long-term follow-up. Foot Ankle1981; 1:279-283.
- Bingold AC: Ankle and subtalar fusion by a transarticular graft. J Bone Joint Surg 1956; 38B:862-870.
- Boyd HB: Indications for fusion of the ankle. Orthop Clin North Am 1974; 5(1): 191.
- Carrier DA, Harris CM: Ankle arthrodesis with vertical Steinmann’s pins in rheumatoid arthritis. Clin Orthop Rel Res 1991; 268:10-14.
- Casadel R, Ruggierl P, Guiseppe T, et al: Ankle resection arthrodesis in patients with bone tumors. Foot Ankle Int 1994; 15:242-249.
- Charnley J: Compression arthrodesis of the ankle and shoulder. J Bone Joint Surg 1951; 33B:180-191.
- Cierney G, Cook G, Mader J: Ankle arthrodesis in the presence of ongoing sepsis. Orthop Clin North Am 1989; 20:709-721.
- Cracchiolo AC: Methods and follow-up statistics on ankle arthrodesis. Clin Orthop 1991; 268:2-111.
- Davis RJ, Mills MB: Ankle arthrodesis in the management of traumatic ankle arthrosis: a long-term retrospective study. J Trauma 1980; 20:674.
- Gellman H, Lenihan M. Halikis N, et al: Selective tarsal arthrodesis: an in-vitro analysis of the effect on foot motion. Foot Ankle 1987; 8:127-133.
- Gilberson RG, Janes JM: Tibiocalcaneal fusion: a surgical technic. Surg Gynecol Obstet 1954; 99:773.
- Gruen GS, Mears DC: Arthrodesis of the ankle and subtalar joints. Clin Orthop Rel Res 1991; 268:15-20.
- Hamsa WR: Panastragaloid arthrodesis. J Bone Joint Surg 1935; 18-A:732-736.
- Hefu FL, Baumann JU, Morscher EW: Ankle joint fusion: determination of optimal position by gait analysis. Arch Orthop Trauma Surg 1980; 96:187.
- Holt RS, Hansen ST, Mayo KA, Sangeorzan BJ: Ankle arthrodesis using internal screw fixation. Clin Orthop Rel Res 1991; 268:21-28.
- Horwitz T: The use of the transfibular approach in arthrodesis of the ankle joint. Am J Surg 1942; 55:550.
- Hunt WS, Thompson HA: Pantalar arthrodesis: a one-stage operation. J Bone Joint Surg 1954; 36-A:349-363.
- Inman TV: The subtalar joint. In the Joints of the Ankle. Baltimore, Williams & Wilkins. 1976, p 37.
- Iwata H, Yasuhara N, Kawashima K, et al: Arthrodesis of the ankle joint with rheumatoid arthritis: experience with the transfibular approach. Clin Orthop 1980; 153:189.
- Jackson A, Glasgow M: Tarsal hypermobility after ankle fusion: fact or fiction? J Bone Joint Surg 1979; 61-A:470.
- King HA, Watkins TB Jr. Samuelson KM: Analysis of foot position in ankle arthrodesis and its influence on gait. Foot Ankle 1980; a:44.
- Kitaoka HB: Salvage of nonunion following ankle arthrodesis for failed total ankle arthroplasty. Clin Orthop Rel Res 1991; 268:37-43.
- Küntscher G: Combined arthrodesis of the ankle and subtalar joints. In Practice of Intramedullary Nailing. Springfield, IL, Charles C. Thomas, 1967. pp 207-209.
- Mann RA: Biomechanics of the Foot and Ankle. In Mann RA, Coughlin MJ (eds): Surgery of the Foot and Ankle, 6th ed. Mosby, Chicago, 1993.
- Marek FM, Schein AJ: Aseptic necrosis of the astragalus following arthrodesing procedures of the talus. J Bone Joint Surg 1945; 27-A:587-594.
- Miller SD, Myerson MS: Tibiotalar arthrodesis. In Myerson MS (ed): Foot and Ankle Clinics, Vol 1. Philadelphia, WB Saunders, 1996, pp 151-162.
- Papa J, Myerson M, Girard P: Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. J Bone Joint Surg 1993; 75-A:1056-1066.
- Papa JA, Myerson MS: Pantalar and tibiotalocalcaneal arthrodesis for post-traumatic osteoarthrosis of the ankle and hindfoot. J Bone Joint Surg 1992; 74-A:1042-1049.
- Quill GE: Subtalar arthrodesis. In Myerson M (ed): Current Therapy in Foot and Ankle Surgery. Chicago, Mosby-Yearbook, 1993.
- Quill GE: Tibiotalocalcaneal and pantalar arthrodesis. Foot Ankle Clin North Am 1996; 1(1):199-210.
- Quill GE: Tibiotalocalcaneal arthrodesis. Techniques Orthop 1996; 11(3):269-273.
- Quill GE: Triple Arthrodesis of the Foot With Autogenous Bone Grafting. Surgery Videotape Library . Rosemont, IL, American Academy of Orthopaedic Surgeons, 1995.
- Reckling FW: Early tibiotalocalcaneal fusion in the treatment of severe injuries of the talus. J Trauma 1972; 12:390-396.
- Russotti GM, Johnson KA, Cass JR: Tibiotalocalcaneal arthrodesis for arthritis and deformity of the hind part of the foot. J Bone Joint Surg 1988; 13:145.
- Soren A, Waugh TR: The historical evolution of arthrodesis of the foot. Int Orthop 1980; 4:3.
- Staples OS: Posterior arthrodesis of the ankle and subtalar joints. J Bone Joint Surg 1956; 38A(1):50-58.
- Steindler A: The treatment of the flail ankle: panastragaloid arthrodesis. J Bone Joint Surg 1923; 5A: 284-294.
- Stuart MJ, Morrey BF: Arthrodesis of the diabetic neuropathic ankle. Clin Orthop 253:209-211, 1990.
- Vahvanen V: Arthrodesis of the TC or pantalar joints in rheumatoid arthritis. Acta Orthop Scand 1969; 40:642-652.



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.