The effectiveness of psychological interventions for the rehabilitation of low back pain: a randomized controlled trial evaluation
Aug 22, 2019Keywords
Low back pain; Educational reconditioning; Physical treatment; Operant conditioning; Relaxation; Biofeedback; Coping skills
Introduction
Chronic pain is a health care problem of considerable importance. Prevalence estimates (Horal 1969; Bonica 1980) suggest that 60% of adults will experience low back pain during a given year and 30% will seek treatment for this problem. Although a substantial number of these cases will resolve satisfactorily (Bergquist-Ullman and Larsson 1975), a minority of perhaps 3-4% become cases of chronic pain and accompanying disability. These numbers translate to staggering costs for health care and disability payments and have led to an increased interest in the rehabilitation of workers with chronic low back pain.
Correspondence to: Elizabeth M. Altmaier, 356 Lindquist Center, University of Iowa, Iowa City, IA 52242, USA.
The most recent area of intervention is the use of treatments predicated on psychological research and theory. This focus on psychological aspects of treatment developed as a result of an increased understanding of pain as a complex phenomenon that comes about through an interaction of sensory-discriminative, motivational-affective, and cognitive-evaluative components (Melzack and Wall 1965). In addition, it has become clear that the communication of pain influences the experience of pain and that pain responses can be altered by environmental factors (Fordyce 1976).
Based on these premises, several psychologically oriented treatments have been used for chronic pain: operant approaches to eliminate pain behaviors, such as prolonged inactivity and over-medication, and to substitute behaviors inconsistent with a sick role: relaxation training, with and without biofeedback adjuncts, to alter the subjective experience of pain; and cognitive-behavioral treatments to teach the patient an array of coping skills and strategies (Turner and Chapman 1982a,b; Linton 1986). These treatments appear to have considerable promise in treating chronic pain, including low back pain. Research suggests that psychological treatments (broadly defined) assist pain patients in reducing medication intake, increasing physical activity, and returning to more normal functioning. However, although research has been promising to date, very few firm conclusions about the effectiveness of any particular treatment have been made.
A recent meta-analysis (Malone and Strube 1988) examined 109 studies which evaluated non-medical treatments for chronic pain with clinical populations. Among these studies were those examining psychological treatments (e.g., biofeedback, cognitive treatments) for back pain. Although a large number of studies were examined, only 48 provided sufficient information to calculate effect sizes. The meta-analysis revealed that psychological treatments were successful when compared to the outcomes of no-treatment control groups. Furthermore, patients who received autogenic training, multicomponent treatments, a pill placebo, or biofeedback training reported the best outcomes. Missing from these results, however, is a longitudinal assessment of outcomes as well as an assessment of patient characteristics associated with favorable outcomes.
The purpose of the present study was to compare patient outcomes of 2 treatment packages: (a) a standard inpatient rehabilitation program for chronic low back pain, which emphasized education and physical reconditioning, and (b) a psychologically based program which added to the standard program components of operant conditioning, relaxation, biofeedback, and coping skills training. Our interest was in whether the psychologically based treatment would enhance patient outcome, assessed along several dimensions of patient functioning, over that demonstrated by the standard rehabilitation program.
Method
Patient population
The study group consisted of patients consecutively admitted over an 18-month period to the Low Back Rehabilitation Program administered through the Spine Diagnostic and Treatment Center, Department of Orthopaedic Surgery, University of Iowa Hospitals and Clinics. In order to be admitted to the program, patients had to meet the following criteria: disabled and not working due to pain for at least 3, but no more than 30, months; not candidates for lumbar surgery; 18-63 years of age; not currently involved in personal injury litigation; not in pain due to pregnancy, severe vertebral fracture, etc.; and not demonstrating significant levels of depression or anger. Forty-seven patients met the eligibility criteria and began the program; 2 patients failed to complete the program and were not included in the data analyses. Patients’ age ranged from 25 to 58 years (mean: 40). Twelve patients were women (26.7%) and 33 were men (73.3%). Eighty percent were married. Education ranged from below high school (13.3%) to high school graduates (37.8%) to completion of vocational/trade school (24.4%) to some college (24.4%). Table I presents the demographic characteristics of the study sample by treatment group.

Treatment programs
The standard treatment program was a multidisciplinary approach to assisting patients in returning to function. Twice daily sessions of physical therapy and daily aerobic fitness training were used to increase activity tolerance levels. Daily education classes taught mechanisms of pain and provided group support. Vocational rehabilitation was included through group educational sessions and an individual counseling session. In addition, patients’ medication intake was monitored so that medication use was aspirin and tylenol only. It should be noted that no patients entered the program using narcotics.
The psychological program ’ built on the standard rehabilitation program in that all patients received the treatment components of the standard program. In addition, several components were added. An operant conditioning component involved daily charting of 2 exercise behaviors (minutes of exercise and number of repetitions) with contingent verbal praise; the chart was displayed on the patient’s room wall. Relaxation training was delivered through daily (1 h) group training sessions and individual practice sessions. Adjunctive biofeedback training was taught in five l-h sessions during the 2nd week. Group and individual training sessions were also used to teach patients an array of cognitive-behavioral coping skills for use with pain. In general, these techniques assisted the patient in reconceptualizing pain as an experience which involves voluntary control over essential elements such as appraisal and pain sensations. In addition to the group and individual sessions, patients completed daily home work exercises which were charted by the patient and reviewed with the treatment group leader on a daily basis.
’ Treatment manuals and patient materials are available on request.
Treatment compliance was assessed in two ways. First, all treatment sessions were audiotaped, and their fidelity to the treatment protocol was evaluated by the first author and an independent rater. Second, all patients’ homework exercise adherence was charted and reviewed by the treatment group leader.
Measures
Three types of “process” measures were used to allow an assessment of the program’s immediate effectiveness in meeting treatment goals. The first, exercise measures, were assessed on all treatment days. The first 3 days were averaged together to yield a beginning level, and the last 3 days were averaged to yield an ending level. Confidence was assessed by a 20-item self-efficacy measure and by the 2-item self-control subscale of the West Haven-Yale Multidimensional Pain Inventory (WHYMPI) (Kerns et al. 1985). Functional aerobic impairment, determined on a stationery bicycle to patients’ symptom or sign limited endpoint, was defined as the ratio of the difference of the age- and sex-predicted aerobic power and the functional work capacity to the predicted aerobic power.
Program “outcomes” were conceptualized on 3 levels: disability, self-reported pain, and life interference. The Low Back Pain Rating Scale (Lehmann et al. 1983) and 2 measures of return to employment were used to assess disability, the McGill Pain Questionnaire (MPQ) (Melzack 1975) assessed self-reported pain, and scores on the Negative Mood and Interference subscales of the WHYMPI (Kerns et al. 1985) were obtained for determination of the effect of pain on the patient’s daily functioning. Outcome measures were administered prior to and at the conclusion of the rehabilitation program, as well as at the 6-month return visit.
Patient disability. The Low Back Pain Rating Scale (Lehmann et al. 1983) is a composite measure of patient disability consisting of physical measures of trunk strength and range of motion, patient’s perceptions of pain and dysfunction (assessed by an activities ques-tionnaire and self-reported pain), and physician’s perception of dys-function based on report of pain and extent of disability. Each of these components is combined by a weighted formula to yield a single overall score. Reliability for the measure (coefficient alpha) was reported by Lehmann et al. (1983) as 0.69, and scores on the scale have been found to be correlated to return to work and improvement during rehabilitation among low back pain patients.
Return to employment. Patients’ return to employment or usual activities (in the case of women who were working in the home) was assessed in two ways. A conservative measure determined whether the patient was fully employed at the same job or an equivalent job. A liberal measure considered the patient as employed if he or she had returned to work part-time, was working full-time or part-time at the same job or at a lower level (“light duty”), or was actively involved in training for a different job.
Self-reported pain. The MPQ (Melzack 1975) was used to assess self-reported pain. The MPQ is a multidimensional measure of pain that involves word descriptors to measure the subjective pain experience, ratings of pain intensity, and drawings of pain location. For the purposes of this study, 2 measures from the MPQ were chosen: Present Pain Intensity (PPI) and Pain Rating Index (PRI). The patient was asked to indicate a number-word combination to de-scribe his or her pain at the present time; the response given by the patient, which can range from 1 (“mild”) to 5 (“excruciating”), was used as the measure of pain intensity. In addition, the patient was asked to select certain word descriptors to describe his/her pain. These descriptors are organized into 16 groups, 10 representing sensory aspects of pain, 5 representing affective aspects, and 1 representing cognitive-evaluative aspects. Patients may select one or more words within each group. The PRI was calculated as the sum of the rank values of all words chosen.
Pain interference. Two scales from the WHYMPI (Kerns et al. 1985) were used to assess the extent to which the patient’s pain affected life activities: Interference and Negative Mood. The Inter-ference scale contains 9 items and measures the degree to which pain interferes with aspects of daily living (i.e., household chores, social activities). Cronbach’s alpha for the scale was reported by Kerns et al. as 0.90, and 2-week test-retest reliability was 0.86. The Negative Mood scale contains 3 items and assesses the patient’s mood during the previous week; its internal consistency was reported as 0.73 and test-retest reliability was 0.69.
Scores on each measure were analyzed with a 2x 3 mixed model analysis of variance (ANOVA) with the treatment group (control vs. psychological) serving as the between-subjects factor and time of assessment (admission, discharge, follow-up) serving as the within-subjects factor. As recommended by O’Brien and Kaiser (1985), the multivariate approach to repeated measures analysis was used. In addition, 2 planned comparisons were conducted. The first compari-son contrasted scores at admission to scores at discharge to assess the immediate effect of the program on the functioning of the patients. A second comparison contrasted scores at discharge to scores from the 6-month follow-up to determine whether improve-ments from the rehabilitation program were maintained. To control for type I error, the significance level was set at 0.025 for each individual planned comparison using the Bonferroni procedure.
Cohen’s (1988) power analysis, based on 42 cases, revealed that we are able to detect a difference between groups that accounts for 13% of the variation of the dependent measure with a power of 0.80. We concluded the present investigation had sufficient power to detect large to moderate treatment effects.
Results
Comparability of treatment groups at admission
To assess the equivalence of the 2 treatment groups before initiation of the rehabilitation program, the demographic characteristics of the control and psycho- logical groups were compared by chi-square and ttests. None of these analyses revealed statistically significant differences between groups in terms of demographic characteristics. Additional analyses were con- ducted to determine if initial differences between the 2 groups on the outcome measures existed at admission. The 2 groups did not differ on the Low Back Pain Rating Scale, the or on WHYMPI scores. In summary, the random assignment of patients to the 2 groups resulted in successfully equating the groups in terms of demographic characteristics and scores on the outcome variables at time of admission.
Process measures
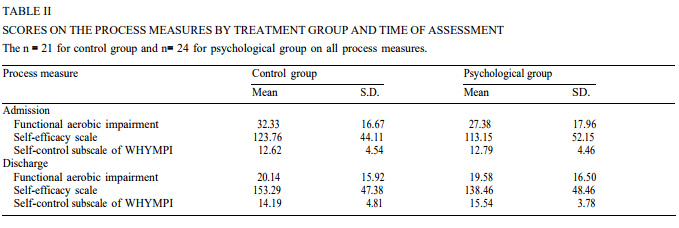
Scores on each process measure were analyzed with a 2 x 2 mixed model ANOVA, with treatment group (control vs. psychological) serving as the between-sub-jects factor and time of assessment (admission vs. dis-charge) serving as the repeated within-subjects factor. It was expected that patients who had received the psychological intervention would exhibit greater imme-diate improvement on each process measure than did those in the control group. Hence, an interaction be-tween treatment group and time of assessment was expected on the process measures. Table II presents means and standard deviations for each process mea-sure, broken down by treatment group and time of assessment.
Exercise measures. Patients engaged in treadmill walking or stationary bicycle ergometer riding during the rehabilitation program. The number of repetitions and minutes on these aerobic exercises were used as indicators of patients’ performance levels. To assess the effectiveness of operant conditioning in enhancing performance levels, the treatment groups were com-pared on these 2 measures separately for the first 3 days and the last 3 days of the program.
As expected, patients in the psychological group (mean: 17.94) completed more repetitions during the first 3 days of the program than did those in the control group (mean: 16.57) (t (29) = 9.73, P < 0.001). Patients in the psychological group (mean: 22.38) also spent more time in aerobic exercises during the first 3 days of the program than did those in the control group (mean: 17.16) (t (26) = 3.45, P < 0.005). During the last 3 days of the program, patients in the psycho-logical group (mean: 60.58) completed more repetitions than did those patients in the control group (mean: 59.29) (t (43) = 2.72, P < 0.009). However, the 2 treat-ment groups did not differ significantly in terms of total minutes spent on aerobic exercises during the last 3 days of the program 53.24; mean psychological ’ 51.79) (t (43) = 0.61, ns). Thus, the operant conditioning received by the psychological group did appear to have enhanced their performance levels on these aerobic exercises.
Functional aerobic impairment. Unexpectedly, analy-sis of functional aerobic impairment revealed only a significant main effect for time of assessment (F (1, 43) = 30.59, P < 0.001). As shown in Table II, patients in both groups showed a decrease in their functional aerobic impairment from admission (mean: 29.69) to discharge (mean: 19.84). The main effect of treatment group was non-significant (F (1, 43) = 0.35, ns) as was the treatment group x time of assessment interaction (F (1, 43) = 1.48, ns). Thus, although the exercise mea-sures revealed the effect of contingent reinforcement, aerobic impairment was not differentially affected.
Confidence and control. For the self-efficacy mea-sure, there was a significant main effect for time of assessment (F (1, 43) = 16.30, P < 0.001) characterized by an overall increase in patients’ ratings of their ability to successfully complete 20 common daily activi-ties despite pain from admission (mean: 118.10) to discharge (mean: 145.38). The main effect of treatment group was not statistically significant (F (1, 43) = 1.00, ns) nor was the predicted interaction between treat-ment group and time of assessment (F (1, 43) = 0.10, ns).
Similar results were observed on the self-control subscale from the WHYMPI. There was a significant main effect of time of assessment (F (1, 43) = 11.45, P < 0.002) but no main effect of treatment group (F (1, 43) = 0.44, ns) or treatment group by time of assess-ment interaction (F (1, 43) = 0.85, ns). Regardless of treatment group, patients showed an increase in their rating of control from admission (mean: 12.71) to dis-charge (mean: 14.91). Thus, the hypothesized influence of coping skills training on confidence was not ob-served.
Outcome measures
Patient disability. ‘Means and standard deviations for the total and subscale scores of the Low Back Pain Rating Scale are presented in Table III. Analysis of the total scores revealed no main effect for treatment group or a group by time of assessment interaction. However, the main effect for time of assessment was highly significant (F (2, 39) = 58.60, P < 0.001). Planned comparisons revealed that patients improved in functioning from admission (mean: 5860) to dis-charge (mean: 69.12) (F (1, 40) = 58.60, P < 0.001) and maintained this improvement at the 6-month follow-up assessment (mean: 67.81) (F (1, 40) = 0.68, ns). Parallel results were obtained for the 3 subscales from the Low Back Pain Rating Scale.
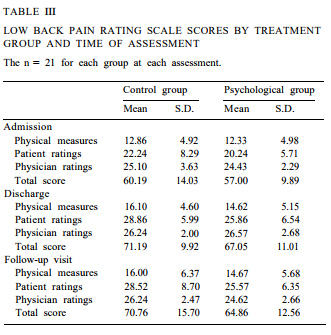
Return to employment. Using the conservative mea-sure, 57.1% of patients had returned to work by the follow-up visit. The difference between the control group (67%) and psychological group (47.6%) was non-significant (1, n = 42) < 1). Using the liberal measure, 81% of patients had returned to work or had made constructive efforts toward re-employment by the 6-month follow-up. Again, the difference between the control group (85.7%) and the psychological group (76.1%) was non-significant (1, n = 42) < 1).
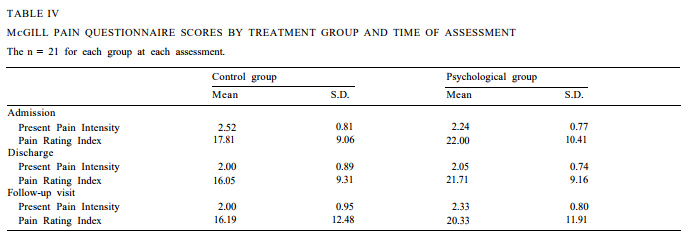
Pain intensity. Table IV presents the means and standard deviations for the PPI and PRI scores from the MPQ. Analysis of PPI scores revealed a significant effect for time of assessment (F (2,39) = 3.74, P < 0.04) and a marginally significant group by time of assess-ment interaction (F (2, 39) = 3.17, P < 0.06). No main effect for treatment group was found. The first planned comparison revealed that patients’ pain intensity de-creased from admission (mean: 2.38) to discharge (mean: 2.02), (F (1, 40) = 7.03, P < 0.02). The second planned comparison showed no significant changes in PPI scores from discharge to the follow-up visit (mean: 2.17) (F (1, 40) = 1.00, ns). To further examine the interaction, protected t tests using the Bonferroni pro-cedure were conducted to compare the 2 treatment groups at each assessment. Analyses revealed no signif-icant differences between the control and psychological groups at admission, discharge, or follow-up (all Ps > 0.05).
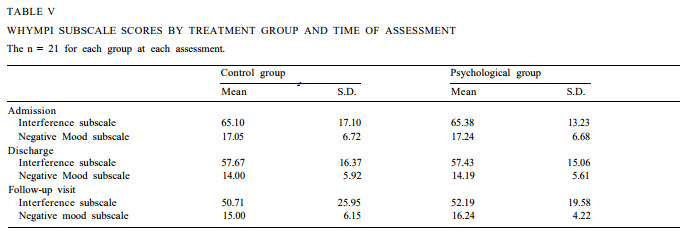
Pain interference. Mean Interference and Negative Mood subscale scores for the 2 treatment groups are shown in Table V, Analysis of the Interference scores indicated a significant main effect for time of assess-ment (F (2, 39) = 15.30, P < 0.001) but neither a signif-icant main effect for treatment group nor an interac-tion between group and time of assessment. The planned comparisons revealed that interference de-creased significantly from admission (mean: 65.24) to discharge (mean: 57.55) (F (1, 40) = 14.57, P < 0.001). In addition, this improvement was maintained at the 6-month follow-up (mean: 51.45) (F (1, 40) = 4.50, ns).
A similar pattern of results was found for the Nega-tive Mood subscale, where a significant main effect for time of assessment was demonstrated (F (2, 39) = 4.60, P < 0.02). The main effect for treatment group and the group by time of assessment interaction were non-sig-nificant. Planned comparisons revealed that patients experienced less affective distress at discharge (mean: 14.10) than at admission (mean: 17.14) (F (1, 40) = 9.37).
Discussion
The results of this study support several general conclusions. First, our analyses of the outcome mea-sures revealed that both treatments were very effective. Patients improved in physical functioning from time of admission to discharge, and they maintained these improvements at the follow-up visit. The interference of pain on patients’ lives and social activities decreased from admission to discharge and remained at this lower level at follow-up. Finally, using a conservative mea-sure, approximately 60% of the patients in the 2 treat-ment programs had returned to work by the follow-up visit. Using a more liberal measure, which credits the patient for part-time work, light duty, or retraining, 81% of the patients had returned to work by the return visit.
Our findings also reveal no significant differences on outcome measures between the treatment groups. All patients improved from admission to discharge and, in most cases, maintained these gains at the time of follow-up. These results suggest that the addition of psychological components (i.e., relaxation training with a biofeedback adjunct, operant conditioning of exercise behaviors, and coping skills training) to the standard rehabilitation program for low back pain patients did not significantly improve the efficacy of the interven-tion. It should be noted that this comparison constituted a stringent test of the psychological components. As our findings clearly indicate, the standard rehabilitation program was quite effective in assisting patients in returning to normal activities. Thus, we were comparing the psychological rehabilitation program to an alternative that was highly efficacious, rather than to a control condition where there was no treatment (e.g., a waiting list control group or patients who were not approved for insurance coverage).
One explanation for the lack of differences between the 2 treatment programs is that both interventions appeared to impact significantly on behavioral change. During the study, several “process” indicators were followed: target exercise behaviors, confidence, and functional aerobic impairment. These indicators re-vealed that both interventions resulted in significant improvements during the program. Thus, the standard program, although not specifically designed to improve these behavioral, cognitive, and physiological pro-cesses, affected these factors to the same degree as the psychological program. Assuming that these processes are important “active ingredients” in improvement manifested by patients during the course of rehabilita-tion, the lack of differential effects of the treatment program is not surprising.
This finding of similar outcomes is further sup-ported by recent reports of treatment effectiveness among chronic low back pain patients. For example, Turner and Clancy (1988) examined the differential effectiveness of an operant behavioral treatment, a cognitive-behavioral treatment, and a waiting list con-trol condition. Their data revealed that both treat-ments resulted in decreased disability, on both physical and psychosocial dimensions, with similar results at a 6- and 12-month follow-up. The lack of differential effectiveness is further supported by a meta-analysis of non-medical treatments for chronic pain (Malone and Strube 1988) which revealed a pattern of uniform effi-cacy of treatments.
Our data and those of related studies appear to suggest that common mechanisms of pain reduction and disability are affected by a number of treatments (see O’Leary et al. 1988). For example, although psy-chological treatments are predicated on the assumption that training in coping skills is the best means of fostering enhanced coping with pain in daily living, it may be true that non-psychological treatments also foster such improvements, albeit in a less targeted manner. An area of future research that is clearly warranted is the examination of mechanisms of change that are commonly affected by a variety of treatments. For example, it may be that any treatment is effective to the degree that it fosters increased confidence and hope in the patient that he or she can deal with pain. A multidimensional conceptualization of the pain ex-perience will assist researchers to better isolate those aspects of pain that are affected by specific treatment components, enabling us to identify the most effica-cious manner of reducing the disability associated with chronic pain.
Acknowledgements
This research was supported by a grant from the National Institute for Handicapped Research (GO0843 5055) to E.M. Altmaier and T.R. Lehmann.
The authors wish to thank Hutha Colby Sayre for assisting with data collection and Dianne Wilkin for leading treatment groups.
References
- Bergquist-Ullman, M. and Larsson, U., Acute low back pain in industry: a controlled prospective study with special reference to therapy and confounding factors, Acta Orthopaed. Scand., Suppl. 170 (1977) 4-117.
- Bonica, J.J., Pain research and therapy: past and current status and future needs. In: L.K.Y. Ng and J.J. Bonica (Eds.), Pain Discomfort and Humanitarian Care, Elsevier, Amsterdam, 1980.
- Cohen, J., Statistical Power Analysis for the Behavioral Sciences, 2nd edn., Erlbaum, Hillsdale, NJ, 1988.
- Fordyce, W.E., Behavioral methods for chronic pain and illness, C.V. Mosby, St. Louis, MO, 1976.
- Horal, J., The clinical appearance of low back disorders in the city of Gothenburg, Sweden, Acta Orthopaed. Scand., Suppl. 18 (1969) entire supplement.
- Kerns, R.D., Turk, D.C. and Rudy, T.E., The West Haven-Yale Multidimensional Pain Inventory (WHYMPI), Pain, 23 (1985) 345-356.
- Lehmann, T.R., Brand, R.A. and Gorman, T.W.O., A low-back rating scale, Spine, 8 (1983) 308-315.
- Linton, S.J., Behavioral remediation of chronic pain: a status report, Pain, 24 (1986) 125-141.
- Malone, M.D. and Strube, M.J., Meta-analysis of non-medical treatments for chronic pain, Pain, 34 (1988) 231-244.
- Melzack, R., The McGill Pain Questionnaire: major properties and scoring methods, Pain, 1 (1975) 277-299.
- Melzack, R. and Wall, P.D., Pain mechanisms: a new theory, Sci- ence, 150 (1965) 971-979.
- O’Brien, R.G. and Kaiser, M.K., MANOVA method for analyzing repeated measures designs: an extensive primer, Psychol. Bull., 97 (1985) 316-333.
- O’Leary, A., Shoor, S., Lorig, K. and Holman, H.R., A cognitive-behavioral treatment for rheumatoid arthritis, Hlth Psychol., 7 (1988) 527-544.
- Turner, J.A. and Chapman, C.R., Psychological interventions for chronic pain: a critical review. I. Relaxation training and biofeed-back, Pain, 12 (1982a) 1-21.
- Turner, J.A. and Chapman, C.R., Psychological interventions for chronic pain: a critical review. II. Operant conditioning, hypnosis, and cognitive-behavioral therapy, Pain, 12 (1982b) 23-46.
- Turner, J.A. and Clancy, S., Comparison of operant behavioral and cognitive-behavioral group treatment for chronic low back pain, J. Consult. Clin. Psychol., 56 (1988) 261-266.
ELIZABETH M. ALTMAIER A, DANIEL W. RUSSELL B, JAMES N. WEINSTEIN C AND CHUAN FENG KAO E
Division of Psychological and Quan tita tit e Foundations and b Center for Health Services Research, College of Medicine, University of Iowa, Iowa City, IA 52242 (USA), ” Spine Diagnostic and Treatment Center, Department of Orthopaedic Surgery, University of Iowa Hospitals and Clinics, Iowa City, IA (USA), d Center for Orthopaedic Excellence, Humana Suburban Hospital, Louisville, KY (USA), and e Department of Psychology, Soochow University (USA)
(Received 4 March 1991, revision received and accepted 20 December 1991)



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.