Cortisone vs. Prp Injections
Aug 22, 2019Melissa T. Parshall, PA-C
A healthy joint requires balance between molecular signals regulating homeostasis, damage, restoration and remodeling. This balance involves balance among different tissues such as cartilage, bone, synovium, ligaments, tendons and menisci. Different factors are able to improve the maintenance of a healthy joint that has been damaged or strained.
What is cortisone? How does it work?
Cortisone is a synthetic version of cortisol, a steroid produced by the body’s adrenal glands. Cortisone medications mimic the action of cortisol but tend to be more powerful. Cortisone injections work by decreasing inflammation. Many patients mistakenly think that cortisone only serves to cover up pain, but that’s not really true. Cortisone can be a very effective method to reduce the inflammation caused by a variety of common orthopedic conditions including tendonitis, bursitis, arthritis and gout. Once the inflammation subsides (3-5 days after injection), pain relief follows.
If the inflammation is severe, or if the inflammation has been around a long time (chronic), the cortisone injection may take longer to take effect and may require more than one injection. Not every patient will respond to a cortisone injection, but the good news is that most people find this to be an excellent treatment for many common inflammatory conditions. If the patient tolerates these injections well, they can safely be repeated every 3-4 months.
What is PRP?
Platelet Rich Plasm is a blood derivative that has a higher platelet concentration than whole blood. When activated, these platelets release proteins and growth factors that promote cellular repair, growth and modulate inflammation. PRP has been used for over 20 years in medicine. Currently, PRP is administered to almost 86,000 athletes in the United States and Europe acute and chronic tendon, ligament and muscle injuries.
How is it used? Indications?
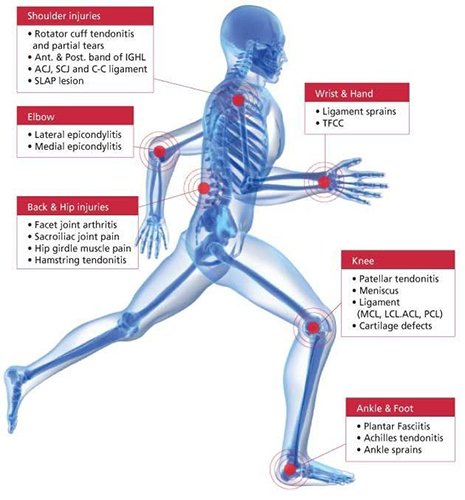
This injection is increasingly being used as a regenerative therapy to treat various tendinopathies. PRP can be used in the treatment of chronic, non-healing tendon injuries including lateral and medial epicondylitis, patella/Achilles/rotator cuff tendons, among others.
The use of PRP in treatment of degenerative knee osteoarthritis has grown over recent years due to high level of safety and ease of administration. Studies have noted that PRP is effective in regards to pain treatment and knee joint function and when compared with hyaluronic acid, the effects last longer (6-12 months).
PRP is safe because it is an autologous products derived from a patient’s’ own blood. There is no risk of rejection or disease and only a very small risk of infection site and donation site. There are no adverse side effects unlike the widely used NSAIDS (Aleve, Advil, Motrin, Ibuprofen, Mobic, Diclofenac) which we know to affect the gastrointestinal, cardiovascular, and renal systems. PRP may not lead to cartilage regeneration, but offers clinical benefit with symptom and function improvement and possibly a slowdown of the degenerative processes.
How does it work? What is the procedure?
PRP therapy uses components of the body’s own blood cells to formulate a customized ‘cocktail” that stimulates the natural healing process in certain orthopedic conditions. The body’s first response to any soft tissue injury is to deliver platelet cells. Filled with healing and growth factors, platelets jump start the repair process and attract the essential aid of stem cells. PRP therapy’s natural healing process magnifies the body’s efforts by delivering a higher concentration of platelets through a simple injection. PRP therapy is associated with reduction in pain and faster healing and has lower risks and lowers costs than surgery.
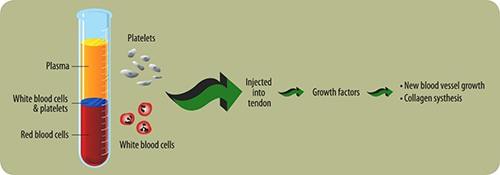 Approximately 15-30mL of venous blood is drawn from patient and collected into a tube. The tube is then centrifuged for 5-15 minutes which separates the blood into 3 distinct layers (platelet poor plasma, red blood cells, and WBC/platelets). The PRP (WBC/platelet layer) is then injected into the affected area on the patient. Rest, depending on pain, and ice are indicated the first 24 hours after the injection. Patients can resume NSAIDS if needed. Up to three injections may be given within a 3-month time frame, usually performed 4 weeks apart. You may, however, gain considerable to complete relief after the first or second injection. The goal of PRP therapy is to resolve pain through healing. Initial improvement may be seen within a few weeks, gradually increasing as the healing progresses. Studies have shown PRP therapy to be effective at relieving pain and returning patients to their normal activities and daily lives. Both ultrasound and MRI images have shown definitive tissue repair after PRP therapy, confirming the healing process. The need for surgery can also be greatly reduced by treating injured tissues before the damage progresses and the condition is irreversible.
Approximately 15-30mL of venous blood is drawn from patient and collected into a tube. The tube is then centrifuged for 5-15 minutes which separates the blood into 3 distinct layers (platelet poor plasma, red blood cells, and WBC/platelets). The PRP (WBC/platelet layer) is then injected into the affected area on the patient. Rest, depending on pain, and ice are indicated the first 24 hours after the injection. Patients can resume NSAIDS if needed. Up to three injections may be given within a 3-month time frame, usually performed 4 weeks apart. You may, however, gain considerable to complete relief after the first or second injection. The goal of PRP therapy is to resolve pain through healing. Initial improvement may be seen within a few weeks, gradually increasing as the healing progresses. Studies have shown PRP therapy to be effective at relieving pain and returning patients to their normal activities and daily lives. Both ultrasound and MRI images have shown definitive tissue repair after PRP therapy, confirming the healing process. The need for surgery can also be greatly reduced by treating injured tissues before the damage progresses and the condition is irreversible.
What is Hyaluronic Acid (HA)?
In your knees, hyaluronic acid is a thick, slippery fluid that helps cushion, lubricate, and protect the bones and joint tissue. With osteoarthritis (OA) of the knee, the HA gets thinner over time and becomes less able to provide protection. HA injections (Euflexxa, Orthovisc, Hyalgan, etc) are used to relieve OA knee pain in people who do not get enough relief from simple pain medications or from exercise and physical therapy. These injections replenish HA, helping provide pain relief. This pain relief has been shown in clinical studies to provide pain relief for up to 6 months. These injections are put directly into your knee to work right at the source of the pain. Treatment consists of 3 injections–1 injection per week for 3 weeks. Some people experience moderate pain relief after the first or second injection, but most people experience significant relief after the third injection. These injections can safely be repeated every 6-12 months as needed.
What is Amniofix?
The use of amniotic tissue has been documented in published literature since the early 1900s. Amniotic membrane has been the subject of many scientific publications evaluating its use in decreasing inflammation and scar tissue and enhancing healing.
Amniotic membrane tissue is donated by healthy consenting mothers undergoing scheduled Caesarean sections. The amniotic membrane is the cover (membrane) surrounding the baby, and is typically discarded after the baby is born. The recovery of the membrane does not affect the baby or the delivery process. Therefore, the donation process does not share the ethical concerns associated with embryonic tissue.
Amniotic tissue contains growth factors which are powerful agents that our bodies produce to signal cells to come to the target site, help the site to heal, and help your own cells regenerate the damaged tissue. Patients who may benefit from this type of injection are those who have been diagnosed with an injury resulting in inflammation, prefer a non-steroidal option, or have failed other conservative therapies.
What are “Stem Cell” procedures?
Adult stem cells are cells from your own body that can renew themselves and turn into other cells (differentiate). They live inside all of us in various tissues, poised to leap into action to repair damage as it occurs. As we age or have big injuries, we may not be able to recruit enough of these cells to the site to fully repair the area. Stem cell procedures help overcome this problem by extracting stem cells from an area of high volume (bone marrow), then concentrating the cells and reinjecting them into the damaged area to help the body heal naturally. The goal is to deliver much greater numbers of stem cells to the injured area than your body can deliver on its own.
Some protocols are a same-day procedure, because the stem cells are harvested and reinjected on the same day. However, for most patients the complete protocol is actually a series of injections that happen over the course of about a week, depending on your unique situation. These injections include a pre-injection of local anesthetic, a same-day stem cell extraction and reinjection procedure.
* Materials borrowed from the American Academy of Orthopaedic Surgeons.
More information can be found at www.aaos.org



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.