Frozen Shoulder
Aug 22, 2019Scott D. Kuiper, M.D.
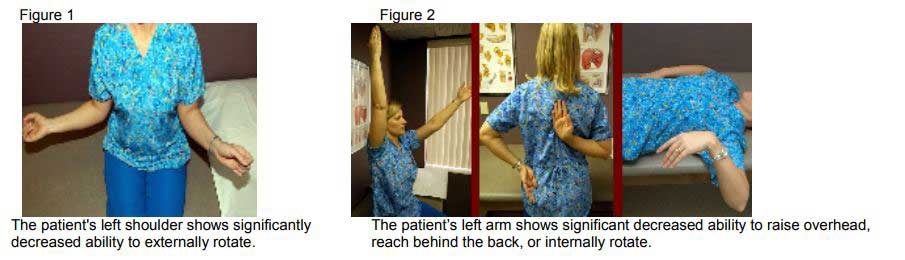
Frozen shoulder is a relatively common condition that effects two to five percent of the population. It generally effects patients between age 40 and 60, and is slightly more common in women than men. Commonly, the patient will present with a gradual onset of pain in the shoulder and they have trouble finding the direct cause of the pain. There is no history of trauma or injury, although the pain is reported during such routine activities as reaching behind them to grab something from the backseat of a car or when reaching back to put on a coat or a shirt. Unfortunately, the pain can cause significant sleep disturbance, and is only mildly relieved by common anti-inflammatory medications, such as Advil or Aleve. Over time, the shoulder becomes stiff and reaching behind one’s back or overhead becomes quite difficult, thus the name frozen shoulder (figure 1, 2). With this history of pain and now stiffness, patients generally present for medical evaluation and treatment. Many times they are seen by their primary care physician who appropriately encourages the use of anti-inflammatory medication and/or starts them on a course of physical therapy, which may help the patient in regards to improving their range of motion and decreasing their pain levels. Unfortunately, some cases are resistant to treatment, and that is when, as orthopaedic surgeons, we see patients with these problems.
Adhesive capsulitis is another term for frozen shoulder, which was coined by Dr. Naviesar in 1945. Adhesive capsulitis has three phases. The first phase is the synovitis or painful phase and can last from 10 to 36 weeks. The second phase is the adhesive phase. During this phase the pain starts to subside, but the stiffness sets in. This can last 4 to 12 months if untreated. The final phase is the resolution phase and can last anywhere from 12 to 42 months with graduated spontaneous improvement.
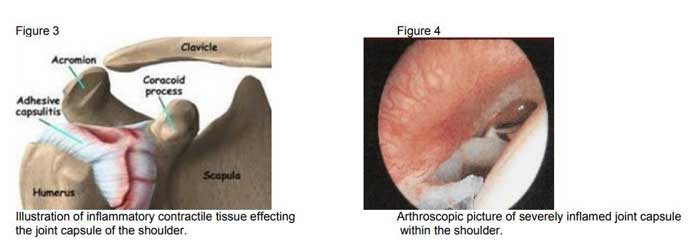
The cause of primary adhesive capsulitis is unknown or idiopathic. It is hypothesized that idiopathic primary adhesive capsulitis is an unusual cellular reaction related to growth factors and other proteins which may stimulate cells to make a protein called collagen, after an inflammatory response, which leads to scarring and contracture of the soft tissues around the shoulder (figure 3). This reaction leads to severe inflammation and swelling within the shoulder, and causes the pain associated with the disease process (figure 4). Secondary adhesive capsulitis can be related to other disease processes, most notably diabetes. Ten to thirty-six percent of diabetic patients are at risk for having a frozen shoulder at some time in adulthood, and these cases can be more resistant to treatment. A frozen shoulder can also be seen and diagnosed after cardiac surgery, cardiac catheterization, breast surgery and even surgery of the shoulder itself.
Fortunately, this problem can be treated successfully. Many times this solely involves nonsurgical treatment modalities. When the patient presents with the type of history noted above, generally a physical examination is performed, plain x-rays are obtained, and sometimes laboratory blood studies are also ordered. Generally the plain x-rays are normal, but they help us rule out other potential problems in the shoulder. Laboratory studies are many times normal as well, but sometimes we see associated positive laboratory values that indicate an underlying inflammatory process. An MRI is sometimes ordered, however, this is usually not to confirm the diagnosis of adhesive capsulitis, but rather to rule out other potential causes of pain in the shoulder such as rotator cuff tear or cartilage injury to the shoulder. Once the diagnosis is confirmed, we try to decide what stage the patient’s frozen shoulder is in. If they are in the early, painful, synovitis phase, a tapering dose of oral prednisone is given along with an injection of cortical steroid in the shoulder to help relieve the severe inflammation. This will generally give quite miraculous relief and allows the patient to start working vigorously on therapeutic exercises to regain any motion that has been lost. Multiple studies and literature support the use of either oral or injectable cortical steroid for treatment of this problem. If the patient presents in the adhesive phase and has moderately restricted range of motion, but not severely restricted range of motion, physical therapy is generally ordered along with the routine use of anti-inflammatory medication. If range of motion is severely restricted, a procedure can be performed to correct this. This procedure is called a manipulation under anesthesia, and does not involve incisions. A numbing shot is given so that the arm is numb and the patient is given a light sedative, and then the shoulder is brought through a range of motion with care so that scar tissue can be broken up allowing the patient to make much more progress in a structured physical therapy program. This has a success rate of 95 percent. A small number of resistant cases will have continued stiffness despite manipulation or they have MRI evidence suggesting other intra-articular pathology and a procedure called an arthroscopic lysis of adhesions can be performed. This procedure involves the use of a pencil-sized arthroscopic camera to view the shoulder with the patient asleep. We can precisely locate the contracted and scarred tissues within the shoulder and release these under direct visualization, which helps restore range of motion to the shoulder.
CONCLUSION
Adhesive capsulitis or frozen shoulder is a condition that involves the gradual onset of pain and stiffness in the shoulder, which can be resistant to treatment such as rest and anti-inflammatory use. Its cause is idiopathic or unknown, although it can be related to other underlying medical conditions, such as diabetes. This generally responds to aggressive physical therapy modalities, as well as the use of oral and/or injectable cortical steroids. In a small number of cases, a procedure called a manipulation under anesthesia or an arthroscopic lysis of adhesions is required for successful treatment.



 Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics.
Our patients can receive MRI imaging onsite at both our Louisville and New Albany Clinics. Providing the latest advances in orthopedic surgery is our specialty.
Providing the latest advances in orthopedic surgery is our specialty. We take a unique, multidisciplinary approach to pain management.
We take a unique, multidisciplinary approach to pain management. Our physical therapists use advanced techniques to help restore strength and mobility.
Our physical therapists use advanced techniques to help restore strength and mobility.  We provide comprehensive, conservative care for a wide variety of foot and ankle conditions.
We provide comprehensive, conservative care for a wide variety of foot and ankle conditions. We offer same- and next-day care to patients with acute injuries.
We offer same- and next-day care to patients with acute injuries. Get back in the game with help from our sports medicine specialists.
Get back in the game with help from our sports medicine specialists.  Our centers are equipped with a state-of-the-art digital X-ray machine.
Our centers are equipped with a state-of-the-art digital X-ray machine.